Session Information
Date: Monday, November 6, 2017
Title: Systemic Lupus Erythematosus – Clinical Aspects and Treatment Poster II: Damage and Comorbidities
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
Systemic lupus erythematosus (SLE) is a chronic disease with varying disease activity levels and morbidities over time; this can affect patients’ health related quality of life (QoL). In clinical practice, we observed substantial heterogeneity in how patients’ QoL evolve over time. This study aims to: 1) Determine if there are latent classes of QoL trajectories (T) among SLE patients as measured by the Medical Outcome Survey Short Form 36 (SF-36) and 2) Identify predictors of different latent class membership.
Methods:
This is a single centre retrospective longitudinal inception SLE cohort. Annual SF-36 has been collected prospectively per clinical protocol. Only patients with ≥3 SF-36 questionnaires, and the 1st must be within 2 years of diagnosis were studied. The primary outcomes are the physical component (PCS) and mental component scores (MCS) of the SF36.
Group based trajectory model was performed using Proc Traj (SAS). One model each was fitted for the PCS and MCS. We tested 2 to 6 class solutions. The best model was determined by a combination of clinical plausibility and statistical criteria: number of patients in each group and model fitting statistic Bayesian Information Criterion (BIC). Models with the lowest BIC and groups containing > 5% of the total sample size were selected as the final models. Predictive effects of baseline variables (listed in table 1) on class membership were tested by logistic regressions.
Results:
171 patients with follow up to 10 years were analyzed. Patient characteristics are represented in table 1.
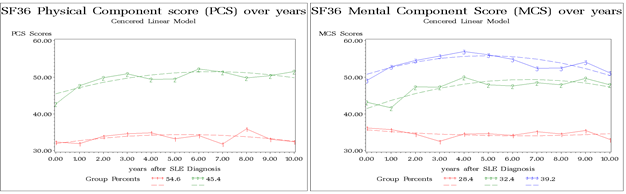
For PCS, 2 classes of T were identified: T1 low PCS with slight improvement over time (54.6%) and T2 persistently very low PCS (45.4%) (Figure 1). For MCS, 3 classes of T were identified: T1 persistently very low MCS (28.4%), T2 low MCS improving over time (32.4%) and T3 average MCS and improving over time (39.2%).
After adjusting for other factors, PCS T2 was significantly associated with older age at SLE diagnosis (OR 0.95 [95% CI 0.92-0.97, p 0.0001]) adjusting baseline disease activity (OR 1.04 [95% CI 0.998-1.09, p 0.06]) and antimalarial treatment (OR 0.36 [95% CI 0.09-1.49, p 0.16]). Regressions did not show significant results for MCS.
Conclusion:
The physical (PCS) and mental health components (MCS) of SF36 follows distinct classes of trajectory in SLE. Some patients have persistently very low PCS and MCS while others show mild improvement from below average to near or above average scores. Younger age at lupus diagnosis was associated with better PCS trajectory (T2).
Figure 1. SF-36 trajectories over time. (A) PCS trajectories and (B) MCS trajectories over time.
|
Table . Patients’ characteristics |
||||||||
|
Factors |
Value |
PCS T1 |
PCS T2 |
p |
T1 |
T2 |
T3 |
p |
|
|
|
n=93 |
n=78 |
|
n=49 |
n=54 |
n=68 |
|
|
Age at SLE diagnosis |
Mean ± SD |
39.57 ± 14.60 |
31.13 ± 10.07 |
<.001 |
34.32 ± 11.33 |
36.65 ± 14.90 |
35.98 ± 13.59 |
0.66 |
|
Gender |
F |
80 (86.0%) |
71 (91.0%) |
0.31 |
45 (91.8%) |
47 (87.0%) |
59 (86.8%) |
0.66 |
|
Ethnicity
|
Asian |
6 (6.5%) |
11 (14.1%) |
0.31 |
1 (2.0%) |
9 (16.7%) |
7 (10.3%) |
0.01 |
|
Black |
17 (18.3%) |
10 (12.8%) |
|
11 (22.4%) |
3 (5.6%) |
13 (19.1%) |
|
|
|
Caucasian |
60 (64.5%) |
47 (60.3%) |
|
35 (71.4%) |
33 (61.1%) |
39 (57.4%) |
|
|
|
Others |
10 (10.8%) |
10 (12.8%) |
|
2 (4.1%) |
9 (16.7%) |
9 (13.2%) |
|
|
|
Secondary school or higher |
Yes |
82 (88.2%) |
72 (92.3%) |
|
44 (89.8%) |
50 (92.6%) |
60 (88.2%) |
|
|
Fibromyaigia |
Yes |
7 (7.5%) |
5 (6.4%) |
0.77 |
6 (12.2%) |
3 (5.6%) |
3 (4.4%) |
0.23 |
|
Baseline_SLEDAI-2K |
Mean ± SD |
9.30 ± 6.54 |
12.06 ± 9.57 |
0.02 |
9.43 ± 7.44 |
10.87 ± 8.60 |
11.13 ± 8.33 |
0.51 |
|
SDI at year 1 |
Mean ± SD |
0.25 ± 0.76 |
0.37 ± 0.79 |
0.29 |
0.35 ± 0.66 |
0.15 ± 0.41 |
0.40 ± 1.02 |
0.19 |
|
Prednisone |
Yes |
81 (87.1%) |
65 (83.3%) |
0.48 |
40 (81.6%) |
45 (83.3%) |
61 (89.7%) |
0.41 |
|
Anti-malarial |
Yes |
89 (95.7%) |
72 (92.3%) |
0.34 |
47 (95.9%) |
51 (94.4%) |
63 (92.6%) |
0.75 |
|
Immunosuppressant s |
Yes |
22 (23.7%) |
21 (26.9%) |
0.62 |
10 (20.4%) |
14 (25.9%) |
19 (27.9%) |
0.64 |
|
All factors are at baseline |
||||||||
To cite this abstract in AMA style:
Fung W, Lim L, Su J, Touma Z. Trajectories of Quality of Life in an Iception Cohort of Lupus Patients and Their Determinants [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/trajectories-of-quality-of-life-in-an-iception-cohort-of-lupus-patients-and-their-determinants/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/trajectories-of-quality-of-life-in-an-iception-cohort-of-lupus-patients-and-their-determinants/