Session Information
Date: Sunday, October 26, 2025
Title: Abstracts: Patient Outcomes, Preferences, & Attitudes (0789–0794)
Session Type: Abstract Session
Session Time: 2:00PM-2:15PM
Background/Purpose: Medication adherence in SLE is suboptimal and contributes to increased disease activity, organ damage, and mortality. Trauma exposure is common among those with SLE and may undermine adherence behaviors by disrupting patients’ sense of stability and future orientation. As a result, trauma-exposed patients may be more likely to focus on immediate needs over long-term planning, reducing the effectiveness of adherence messaging centered on future outcomes such as flare prevention or organ preservation. Resilience—the capacity to adapt to adversity—may buffer these effects. However, the relationship between trauma, resilience, and medication adherence in SLE remains underexplored.
Methods: We conducted a cross-sectional study of patients with SLE (2012 SLICC or 2019 ACR/EULAR criteria) enrolled in an academic lupus registry. The extent of and reasons for nonadherence were measured by the DOSE-Nonadherence-SLE. Patients also completed the polysymptomatic distress (PSD) scale, the Brief Resilience Scale, and the Trauma History Screen. Rheumatologists assessed SLE activity using the Physician’s Global Assessment (PGA). Trauma exposure history was categorized into abusive (physical, sexual, and emotional trauma as an adult or child), non-abusive, or no trauma. We used Fisher’s exact test, Chi-squared test, and Wilcoxon rank sum test for group comparisons and multivariable regression models to examine the association between trauma exposure and medication nonadherence, including an interaction term for resilience.
Results: Among 238 patients (median age 42, 92% female, 36% White, 57% Black, 6% Hispanic), 111 (47%) reported nonadherence, 98 (41%) reported abusive trauma, and 101 (42%) reported non-abusive trauma. Nonadherent patients were more likely to be younger, identify as Black or Other race or Hispanic ethnicity, have higher symptom severity scores, and report a history of abusive trauma (Table 1).In adjusted models, abusive trauma was associated with 58% higher risk of nonadherence compared to no trauma (Table 2). Black and Other race and Hispanic ethnicity also remained significantly associated with nonadherence. Resilience moderated the relationship between trauma and medication nonadherence (p=0.02); patients with abusive trauma as well as low resilience had the highest risk of nonadherence.Nonadherent patients with abusive trauma, compared to those with non-abusive trauma or no trauma, more frequently reported missing SLE medications because “I am tired of taking medicines every day,” “I feel that nothing will get better even if I take them,” and “I felt too sick.” They were less likely to report “I could not fill the medicines on time.” (Table 3)
Conclusion: Abusive trauma was common and independently associated with greater risk of medication nonadherence in SLE, and resilience was a protective moderator. Patients with abusive trauma tended to endorse motivational barriers to adherence but were less likely to endorse difficulty filling medicines on time. These findings underscore the importance of trauma-informed, resilience-enhancing approaches to improve medication adherence for trauma-exposed patients.
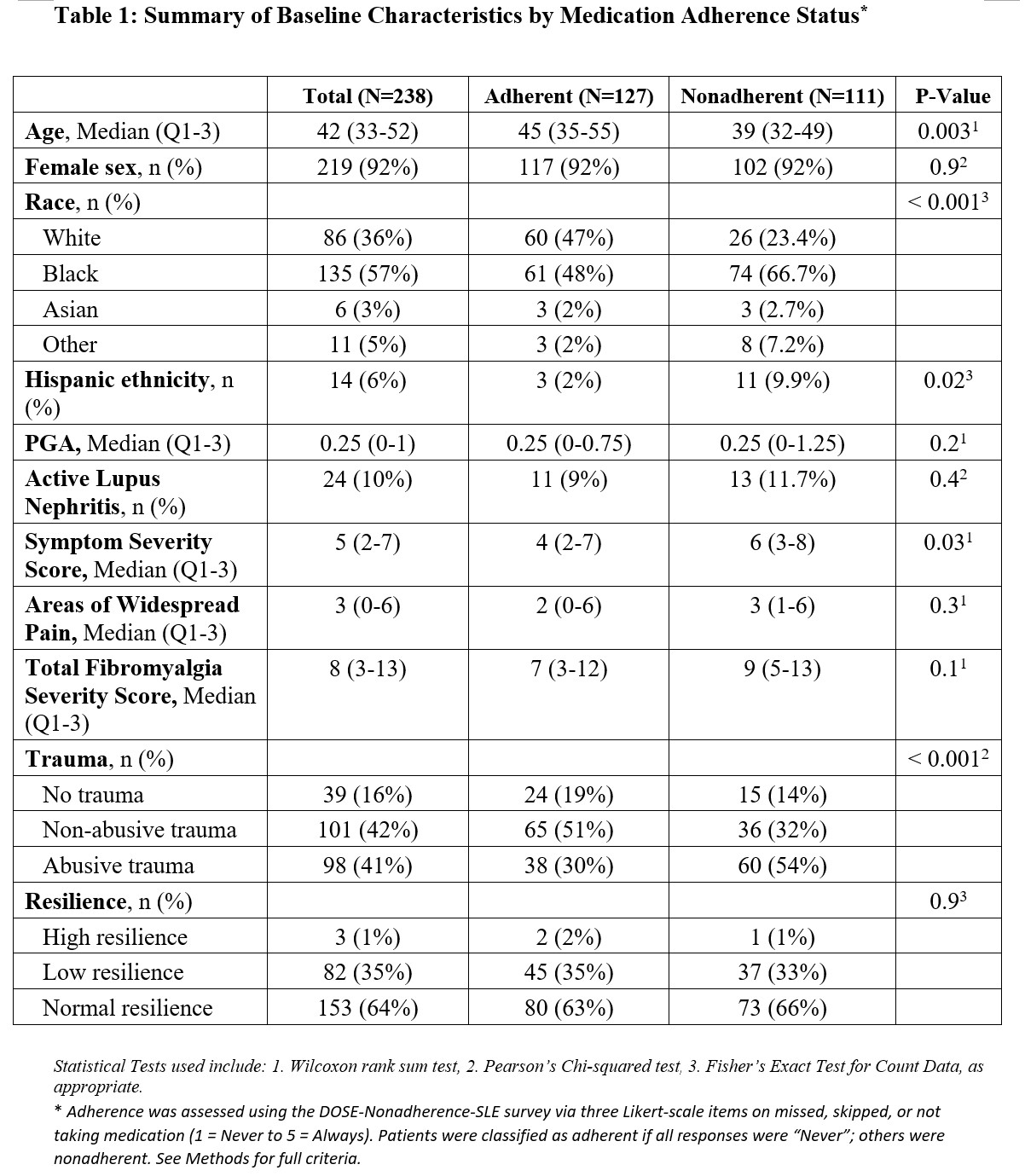 Table 1: Summary of Baseline Characteristics by Medication Adherence Status
Table 1: Summary of Baseline Characteristics by Medication Adherence Status
.jpg) Table 2: Association between Trauma and Medication Nonadherence
Table 2: Association between Trauma and Medication Nonadherence
.jpg) Table 3: Reasons for nonadherence based on the DOSE-Nonadherence-SLE by trauma history.
Table 3: Reasons for nonadherence based on the DOSE-Nonadherence-SLE by trauma history.
To cite this abstract in AMA style:
Sun K, Pozsonyiova S, Eudy A, Clowse M, Sadun R, Maheswaranathan M, Doss J, Harris N, Criscione-Schreiber L, Drake C, Somers T, Snyderman R, Rogers J. The weight of the past: how trauma and resilience shape medication adherence in SLE [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/the-weight-of-the-past-how-trauma-and-resilience-shape-medication-adherence-in-sle/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-weight-of-the-past-how-trauma-and-resilience-shape-medication-adherence-in-sle/
