Session Information
Date: Monday, October 22, 2018
Title: Spondyloarthritis Including Psoriatic Arthritis – Clinical Poster II: Clinical/Epidemiology Studies
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with psoriatic disease (PsD) are at a high risk of developing cardiovascular events (CVE). The performance of clinical algorithms for cardiovascular risk stratification, such as the Framingham Risk Score (FRS), is sub-optimal in this patient population. The study aims were: 1) to assess whether subclinical atherosclerosis, as evaluated by carotid ultrasound, could predict future CVE in patients with PsD and 2) to determine whether incorporation of imaging data could improve the prediction of CVE beyond clinical cardiovascular algorithms.
Methods: Patients with PsD from a large longitudinal cohort underwent ultrasound assessment of the carotid artery at baseline. The extent of atherosclerosis was assessed using mean carotid intima media thickness (cIMT in µm) and total plaque area (TPA in cm2). Patients were followed according to a standardized protocol at 6-12 month intervals. Incident CVE that occurred following the ultrasound assessment were identified from the cohort database and through linkage with national hospitalization and death registries. A cardiologist reviewed the medical records related to each CVE and classified them to major CVE (myocardial infarction, stroke, revascularization or cardiovascular death) and minor CVE (angina, TIA, CHF exacerbation). The association between measures of carotid atherosclerosis and the risk of developing future CVE was evaluated using Cox proportional hazard models after adjusting for FRS categories.
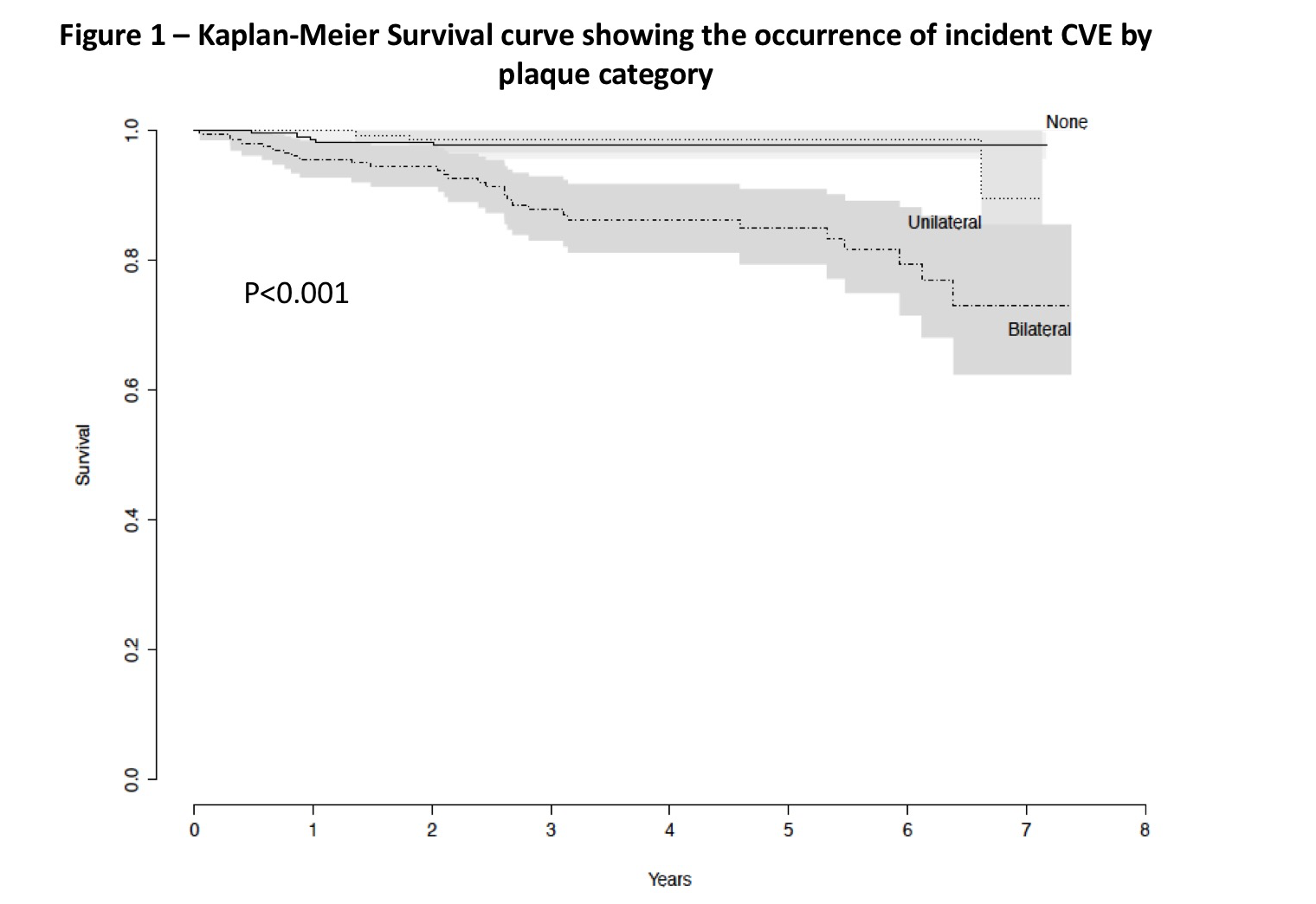
Results: Overall, 607 patients with PsD (66.7% with PsA) were assessed and 37 patients developed incident CVE confirmed by the cardiologist (28 major CVE). Their mean age was 57.1 (SD 11.7) and 57.7% were males. 26% and 34.8% had unilateral and bilateral carotid plaques, respectively. The incidence rate of CVE was higher in patients with bilateral carotid plaques compared with unilateral/no plaques (3.96 vs. 0.54 events per 100 person years; p<0.001, Figure 1).
In multivariable regression models, TPA (Hazard Ratio (HR) 2.20, 95% Confidence Interval (CI) 1.51, 3.22; p <0.001), mean cIMT (HR 1.21, 95% CI 1.08, 1.34; p<0.001) and bilateral carotid plaques (HR 2.89, 95% CI 1.07, 7.77, p=0.03) predicted incident CVE after controlling for FRS. The results were similar after restricting the analysis to patients with major CVE and after excluding patients with a history of CVE at baseline.
Conclusion: Patients with PsD with subclinical carotid atherosclerosis are more likely to develop future CVE. Carotid ultrasound could potentially improve the identification of patients with PsD who are at high cardiovascular risk.
|
Table 1- The association between subclinical atherosclerosis and incident cardiovascular events (N=607, 37 events) – Cox proportional hazard model |
||||
|
|
Univariate analysis
|
Adjusted for Framingham risk score
|
||
|
|
HR (95% CI) |
P value |
HR (95% CI) |
P value |
|
TPA |
3.48 (2.54, 4.79) |
<0.0001 |
2.20 (1.51, 3.22) |
<0.0001 |
|
Mean IMT |
1.37 (1.25, 1.51) |
<0.0001 |
1.21 (1.08, 1.34) |
0.0009 |
|
Max IMT |
1.19 (1.12, 1.26) |
<0.0001 |
1.11 (1.03, 1.19) |
0.003 |
|
Plaques Unilateral vs. none Bilateral vs. none |
0.84 (0.20, 3.50) 6.82 (2.64, 17.62) |
0.81 <0.0001 |
0.57 (0.14, 2.38) 2.89 (1.07, 7.77) |
0.44 0.03 |
|
CI- confidence interval, HR- hazard ratio, IMT- intima media thickness, TPA – total plaque area |
||||
To cite this abstract in AMA style:
Sobchak C, Akhtari S, Harvey P, Gladman DD, Chandran V, Cook RJ, Eder L. The Value of Carotid Ultrasound in Cardiovascular Risk Stratification in Patients with Psoriatic Disease [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/the-value-of-carotid-ultrasound-in-cardiovascular-risk-stratification-in-patients-with-psoriatic-disease/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-value-of-carotid-ultrasound-in-cardiovascular-risk-stratification-in-patients-with-psoriatic-disease/