Session Information
Date: Monday, November 11, 2019
Title: Epidemiology & Public Health Poster II: Spondyloarthritis & Connective Tissue Disease
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Associations between ulcerative colitis (UC) and Crohn’s disease, known together as inflammatory bowel disease (IBD), with axial pain, inflammatory back pain (IBP) and spondyloarthritis (SpA) are well described but vary among studies. This study presents previously unreported nationally representative data from the US health surveys NHANES 2009-10 and NHANES II (1976-80) comparing axial pain rates in those with and without IBD.
Methods: NHANES 2009-10 and NHANES II questionnaires asked patients about history of clinician diagnosed UC (both) or Crohn’s (NHANES 2009-10 only), gastrointestinal symptoms, medical care and IBD comorbidities. Both surveys asked questions about the timing and anatomical distribution of axial pain of at least 3 months and history of clinician-diagnosed arthritis. NHANES 2009-10 also asked questions about pain quality to estimate IBP prevalence (Calin, ESSG, Rudwaleit et al. criteria). Statistical analysis used SASTM 9.4 using survey design variables and sample weights to produce nationally representative estimates.
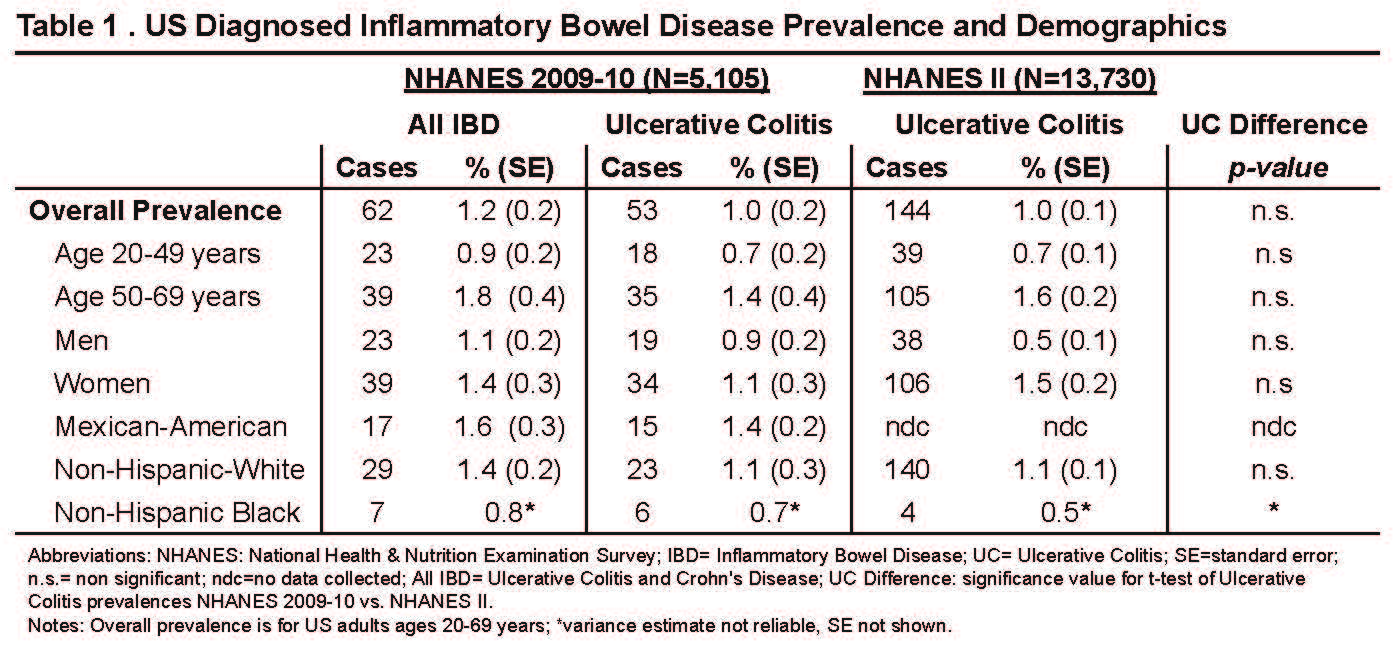
Results: Data for 5105 participants in NHANES 2009-10 and 13,730 in NHANES II ages 20-69 was analyzed. Overall, IBD prevalence in NHANES 2009-10 was 1.2 % (95% CI 1.0-1.4%); UC prevalence was 1.0% (95% CI 0.8-1.2%). UC prevalence in NHANES II was 1.0% (95% CI 0.8-1.2%). In NHANES II, UC rates were higher at ages 50-69 than at ages 20-49 (p< 0.01), and higher among women than men (p< 0.01). (Table 1) In NHANES 2009-10, 69% of IBD cases (Crohn’s or UC) had colonoscopy at diagnosis; 60% had recent gastrointestinal symptoms; 30% had been hospitalized in the previous year or had prior transfusions; and 21% had IBD comorbidities (uveitis, ankylosing spondylitis, colon cancer, osteoporosis).
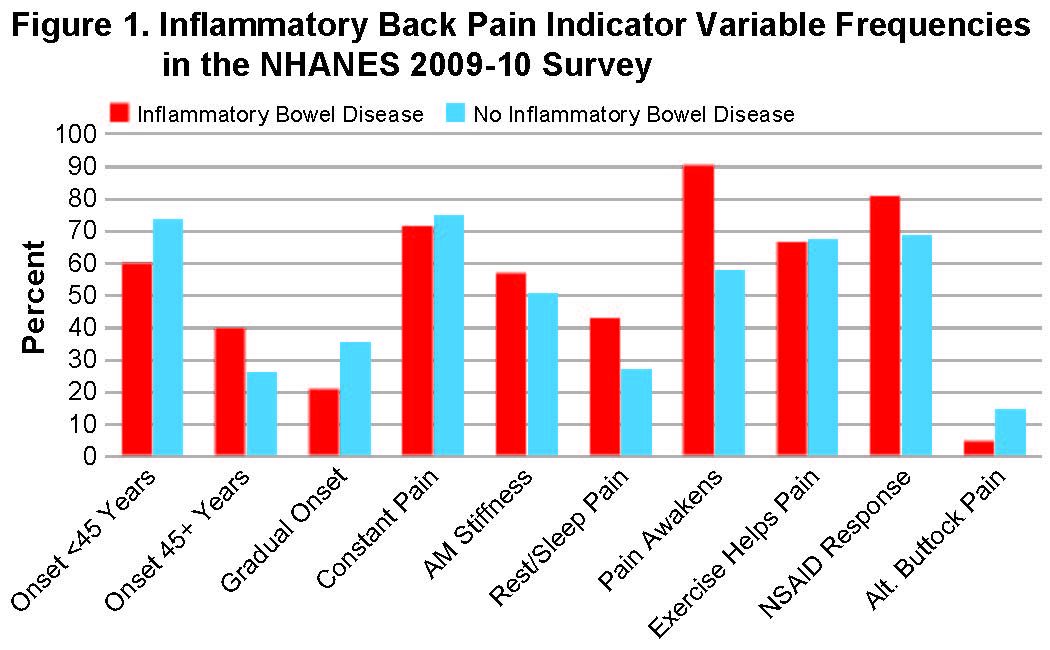
Figure 1. illustrates NHANES 2009-2010 subjects with at least 3 months of back pain. IBD cases were more likely to have pain onset older than 45 years (40.0% vs 26.2%), rest or sleep pain (42.9% versus 27.3%), and pain on awakening (90.5% vs 58.0%).
Figure 2. reveals prevalence of axial pain in IBD patients from both surveys. Prevalence rates of axial pain for at least 3 months were non-significantly increased among IBD cases in NHANES 2009-10 (27.8% vs 19.2%), and increased among UC cases in NHANES II (22.3% vs. 7.8%; p< 0.01). Amor Criteria axial pain (axial pain plus pain at night or AM stiffness) was increased among UC cases in the NHANES II data (21.3% vs 7.4%, p< 0.01), as was clinician-diagnosed arthritis (38.5% vs 20.7%, p< 0.01). IBP and SpA analysis in NHANES 2009-2010 was limited due to sample size so statistical testing wasn’t performed, however, the unadjusted overall IBP and SpA estimates for IBD cases was 9.7% and 10% respectively, vs. 7.2% and 1.8% of controls.
Conclusion: Prevalences of UC in these two nationally representative population surveys were consistent at 1% of the general population, similar to previous surveys. This suggests stable UC prevalence and recognition rates between the 2 survey time periods. Chronic axial pain history was seen in almost 25% of IBD and UC cases and arthritis diagnosis rates were increased. IBD-axial pain was more likely to have an older age at onset and to occur with sleep or rest. Studies with larger sample sizes are required to estimate IBP and SpA rates in IBD.
To cite this abstract in AMA style:
Stens O, Dillon C, Miller F, Weisman M. The US Prevalence of Inflammatory Bowel Disease and Associated Axial Pain: Data from the National Health & Nutrition Examination Survey (NHANES) [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-us-prevalence-of-inflammatory-bowel-disease-and-associated-axial-pain-data-from-the-national-health-nutrition-examination-survey-nhanes/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-us-prevalence-of-inflammatory-bowel-disease-and-associated-axial-pain-data-from-the-national-health-nutrition-examination-survey-nhanes/