Session Information
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Psoriatic arthritis (PsA) occurs in up to 30% of patients with psoriasis (PsO), and usually follows the development of PsO by an average of 7-10 years. However, there is significant variability in the timing of transition from PsO to PsA which contributes to delays in diagnosis and high rates of undiagnosed PsA. In this study, we aim to identify clinical and demographic features associated with the time to transition from PsO to PsA.
Methods: In our longitudinal psoriatic disease cohort, we identified patients with PsO and PsA diagnoses. Time between PsO and PsA diagnoses was calculated as number of years between the 2 diagnoses dates, and were modeled as a continuous outcome variable using multivariable linear regression. Candidate predictors included: gender, age at PsO diagnosis, family history of PsO, BMI, treatment, cardiovascular disease, hypertension, diabetes, dyslipidemia, nail involvement, DLQI, elevated ESR/CRP, alcohol and smoking. A subgroup model was built using patients with BSA data, and using a subset of predictors including age at PsO diagnosis, smoking, elevated ESR/CRP, BMI, family history of PsO and % body surface area (BSA). Model results were presented using coefficient estimates and respective 95% confidence intervals. Variables were ranked based on their relative contribution to the models, as assessed by AIC increase upon removal of the variable from the full model. All tests were two-sided, assuming an alpha level of 0.05.
Results: Our analysis cohort included 384 patients. The median age at PsO diagnosis was 30.4 years, and 52.2% of patients were female. Age at Diagnosis of PsO is statistically significantly associated with transition time from PsO to PsA. Patients aged 42.6 years (Q3) have on average around 12 years less between PsO to PsA compared to patients aged 18.9 years (Q1), after controlling for relevant variables in the model (-11.88 (-13.64, -10.12); p < 0.001). Patients on bDMARD have on average 4.5 years less between PsO to PsA compared to patients on NSAID only, after controlling for other variables in the model (-4.52 (-8.3, -0.74), p = 0.02). Although the use of bDMARDs appears to show a trend towards less years (4.5 yrs) compared to non bDMARDs, the overall effect of treatment was not statistically significant. Patients with BSA of 5% (Q3) have on average 1.1 years more (more number of years) from PsO to PsA compared to patients with BSA of 0.5% (Q1), after controlling for other variables in the model (1.11 (-0.44, 2.65), p = 0.16), though the overall effect of BSA is not significant. Age at PsO diagnosis contributed the most to the model according to the Akaike Information Criterion (AIC). AIC >= 2 justifies statistically improved model, which means it is beneficial to include age in the model.
Conclusion: Our study demonstrated that age of psoriasis onset is important predictor of time to transition from psoriasis to psoriatic arthritis. Patients diagnosed with PsO at an older age have a shorter interval before they develop PsA. The time difference is clinically significant; compared to younger patients (18.9 years, Q1), older patients (42.6 years, Q3) develop PsA on average 12 years sooner. These results suggest that older patients diagnosed with PsO may benefit from earlier screening for PsA.
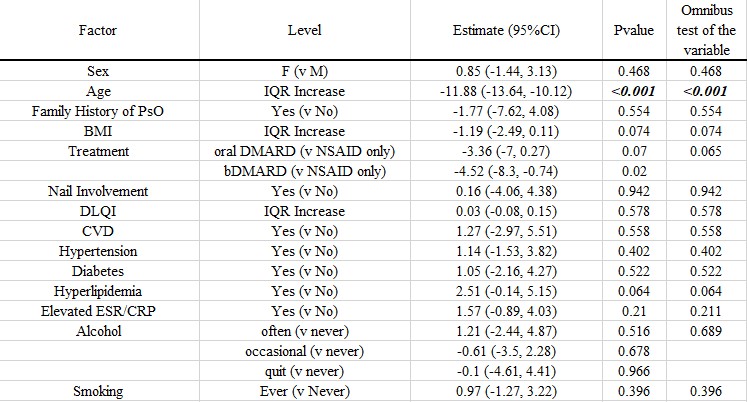 Table 1: Linear Regression Analysis for Time between PsO and PsA Diagnoses
Table 1: Linear Regression Analysis for Time between PsO and PsA Diagnoses
 Figure 1: Ranking of Predictors for Time between PsO and PsA Diagnoses
Figure 1: Ranking of Predictors for Time between PsO and PsA Diagnoses
To cite this abstract in AMA style:
Cheemalavagu S, Jin Y, Husni E. The Transition to Psoriatic Arthritis: What Factors Predict a Shorter Transition from Psoriasis to Psoriatic Arthritis? [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/the-transition-to-psoriatic-arthritis-what-factors-predict-a-shorter-transition-from-psoriasis-to-psoriatic-arthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-transition-to-psoriatic-arthritis-what-factors-predict-a-shorter-transition-from-psoriasis-to-psoriatic-arthritis/
