Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Hemophagocytic lymphohistiocytosis (HLH) is an aggressive and life-threatening syndrome of disordered immune activation marked by excessive inflammation. Immunosuppression remains the mainstay of therapy after targeting the underlying trigger. Both the diagnosis and management of HLH remain challenging, as the disease can mimic a wide spectrum of clinical disorders and immunosuppression can become delayed. A multidisciplinary approach is crucial for the early diagnosis and treatment of this disorder to help improve outcomes. The aim of our study is to explore the relation between time to sub-specialty consultation, HLH consideration and immunosuppression initiation with 30-day mortality.
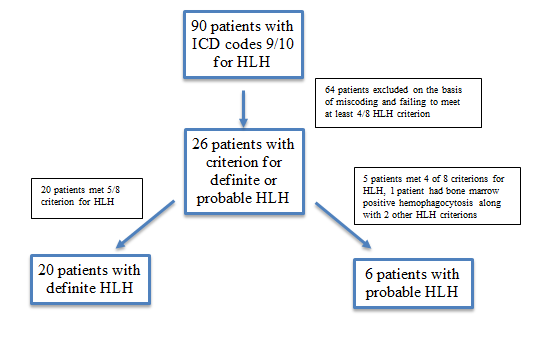
Methods: We performed a retrospective chart review of HLH patients’ age >18 years identified in the electronic medical records by ICD 9/10 coding for HLH and confirmed by chart review. Patients were characterized as having definitive HLH (defined as meeting 5/8 parameters according to the 2004 HLH diagnosis criteria) and probable HLH (defined as meeting 4/8 parameters on the HLH criteria or if they had hemophagocytosis on biopsy). Patients with incomplete clinical data and those not meeting criteria for definitive or probable HLH were excluded. Clinical demographics, underlying etiology, HLH parameters, hospital day of HLH as a diagnostic consideration, time to sub-specialty consultation (rheumatology, allergy/immunology, hematology/oncology, infectious disease, and critical care), hospital day of immunosuppression initiation and 30-day mortality were identified. Student’s t-test was used for comparison of continuous variables.
Results: During the study period, we identified 90 patients with HLH based on ICD coding. After excluding 64 patients based on insufficient clinical data for diagnosis of HLH, 20 patients were identified as having definitive HLH and 6 patients were identified as having probable HLH (Figure 1). Majority of patients 15/26 (58%) were males with a mean (SD) age of 42 (18). Infection (46%) was the most common secondary cause for HLH with 6/11 (54%) as viral etiologies. Corticosteroids were the preferred first line immunosuppressive therapy in all patients. The 30-day mortality in our cohort was 7/26 (27%). The mean (SD) time to any sub-specialty consultation was 1.8 days (1.2) in patients who survived and 3 days (2.3) in patients who died (p=0.23). The mean (SD) time lag from admission to HLH consideration was 6.7 (5.3) vs. 4.6 (3.6) (p=0.26), while the mean (SD) time lag from consideration of HLH to immunosuppression was 2 days (2.7) vs. 8.4 days (8.8) SD (p=0.10) in patients who survived and died respectively.
Conclusion: Among adult patients with definitive or probable HLH seen at a single center, we did not find a statistical significant association between time to sub-speciality consultation, time lag to immunosuppression, and mortality. Our study was not adequately powered to detect small differences and future larger studies are warranted, so appropriate interventions can be developed.
To cite this abstract in AMA style:
Patel S, Ayesha B, Broder A, Gendlina I, Murakhovskaya I, Ramesh M, Balagula Y, Kumthekar A. The Time Lag – the Race in Diagnosis and Management of Hemophagocytic Lymphohistiocytosis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-time-lag-the-race-in-diagnosis-and-management-of-hemophagocytic-lymphohistiocytosis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-time-lag-the-race-in-diagnosis-and-management-of-hemophagocytic-lymphohistiocytosis/