Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Psoriatic arthritis is a chronic inflammatory disease. More than 20% of patients with PsA patients suffer from fibromyalgia, a chronic pain syndrome characterized by widespread pain and tender points. PsA patients with concomitant fibromyalgia have high scores of disease activity, irrespective of underlying inflammatory process. Thus, assessment of clinical disease activity in those patients is challenging. Ultrasound (US) is a common imaging modality for disease activity evaluation. Hence, the aim of the current study is to examine whether US can be used as an objective tool for assessment of disease activity in PsA patients with fibromyalgia.
Methods: The study population included consecutive PsA patients that were recruited prospectively. All the patients fulfilled the CASPAR criteria. The assessment of the patients included complete medical history and physical examination, including assessment of 68 joints, enthesitis (Leeds and SPARCC) and fibromyalgia tender points. All the patients were assessed by the widespread pain index (WPI) and symptom severity score (SSS) for fibromyalgia. Patients were classified with fibromyalgia if they fulfilled the 1990 or 2010 classification criteria for fibromyalgia. All the patients underwent a detailed US evaluation including 40 joints, 40 tenosynovitis and 14 points of entheses (according to the MASES index plus bilateral lateral epicondyles). The score of the US was based on the summation of semi-quantitative score (0-3) for joints and tendons plus enthesitis score based on the MASEI score. Both clinical and sonographic evaluation occurred in the same day and the sonographer was blinded to the clinical data.
Results: Eighty-six patients completed the study. Overall, 3440 joints, 3440 tendons and 1204 entheses were scanned by the US. Thirty-three patients (38%) classified with both PsA and fibromyalgia were compared to 53 (62%) PsA patients without fibromyalgia. The demographic data were overall similar in PsA patients with and without fibromyalgia (Table 1). Patients with PsA and fibromyalgia had significantly increased scores for almost all the clinical measures, including not being in MDA (97% vs 56.6%, p< 0.001), CPDAI (11.5 vs. 7.3, p< 0.001) and DAPSA (33.6 vs. 15.5, p< 0.001). The total US score were similar between patients with and without fibromyalgia. Furthermore, the subcategories of US synovitis, tenosynovitis and enthesitis were comparable in both groups (Table 2).
Conclusion: While patients with PsA and fibromyalgia had increased scores of clinical measures of disease activity compared to those without fibromyalgia, US scores were similar between the groups. Hence, US can be used as a discriminative tool for objective assessment of disease activity in patients with PsA and concomitant fibromyalgia.
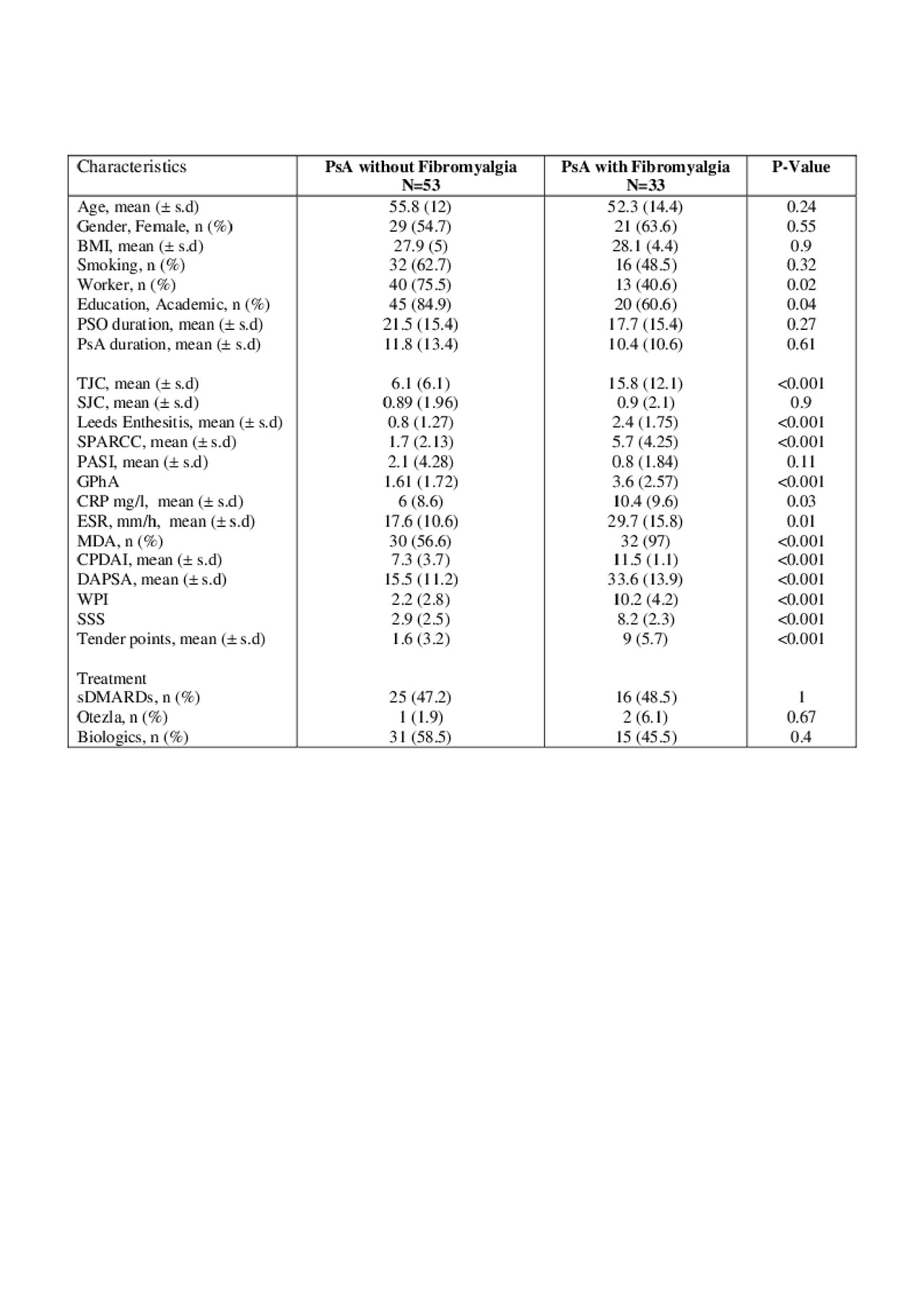
Table 1, Demographic and clinical data
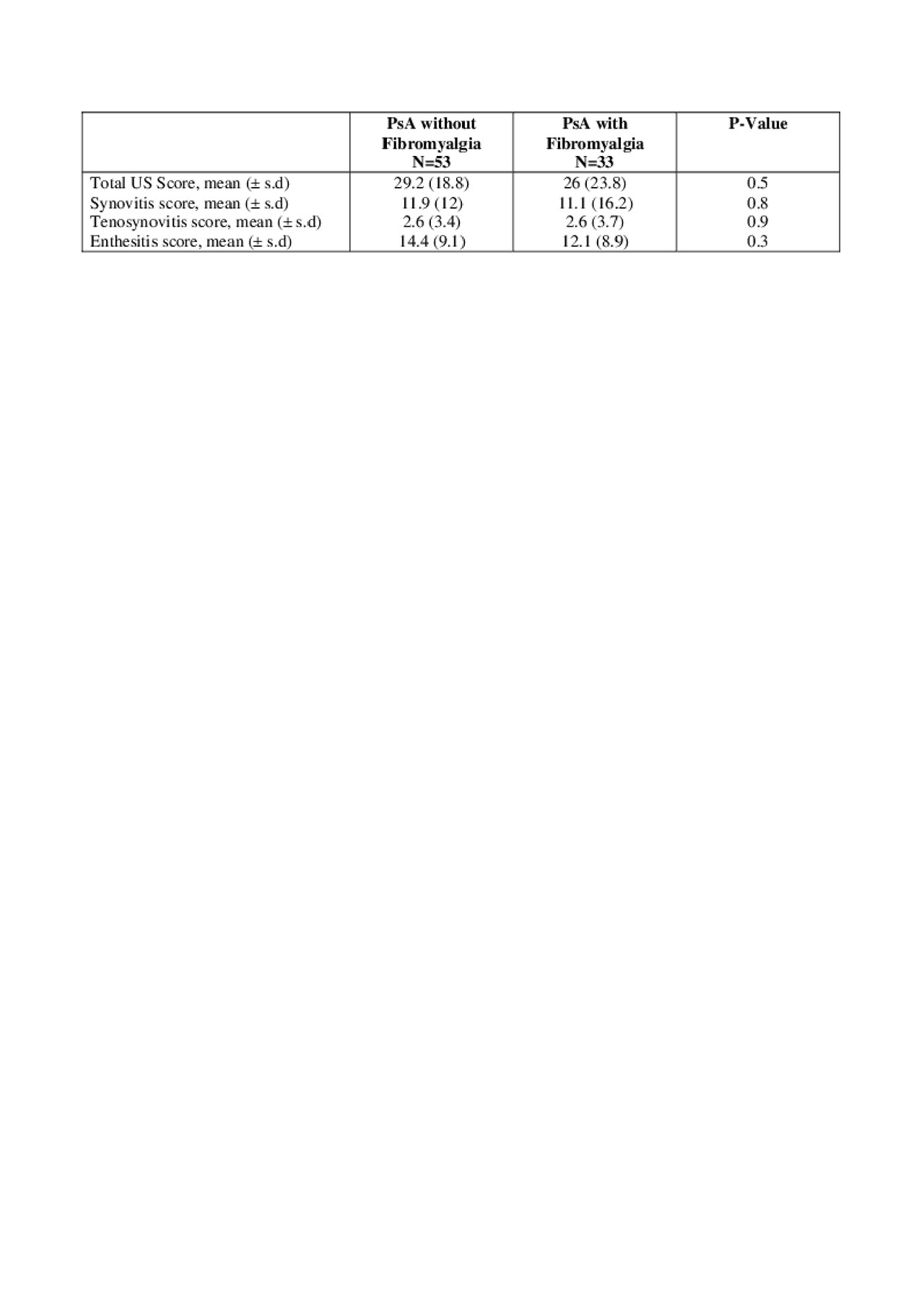
Table 2. Sonographic comparison between PsA with to without fibromyalgia
To cite this abstract in AMA style:
Polachek A, Furer V, Zureik M, Nevo S, Mendel L, Levartovsky D, Wollman J, Aloush V, Berman M, Kaufman I, Lahat Y, Sarbagil-Maman H, Borok S, Broyde A, Eder L, Paran D, Elkayam O. The Role of Ultrasound for the Assessment of Psoriatic Arthritis Patients with Fibromyalgia – Interim Analysis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-role-of-ultrasound-for-the-assessment-of-psoriatic-arthritis-patients-with-fibromyalgia-interim-analysis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-role-of-ultrasound-for-the-assessment-of-psoriatic-arthritis-patients-with-fibromyalgia-interim-analysis/
