Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: The potential impact of psoriatic arthritis (PsA) and rheumatoid arthritis (RA) on the risk of incident diabetes remains unclear. Studies have shown that patients with psoriasis have an increased risk of incident diabetes; however, no published data are available specific to patients with psoriatic arthritis. Furthermore, there is a scarcity of data on the risk of diabetes among patients with rheumatoid arthritis, and the available data in RA are conflicting. We aimed to evaluate the risk of incident diabetes in PsA and RA in the general population, with adjustment for body mass index (BMI) and lifestyle factors.
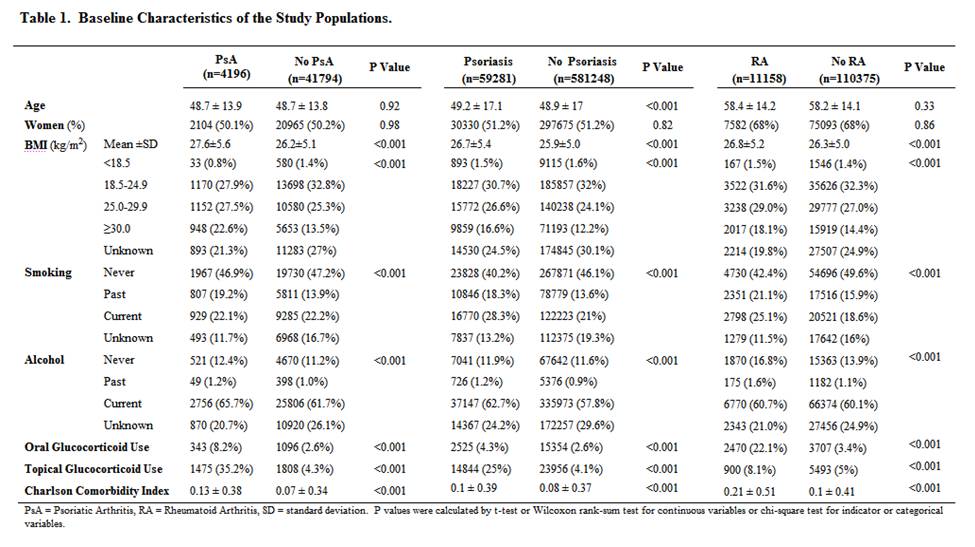
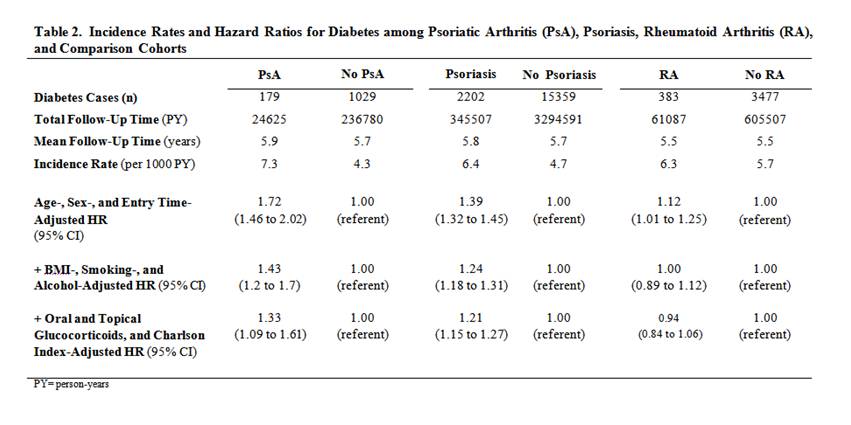
Methods: We conducted a cohort study using data from an electronic medical records database representative of the UK general population, collected between 1986 and 2010. We used previously published definitions of PsA, psoriasis, RA (exposures) and diabetes (outcome) in the same cohort context. We estimated hazard ratios (HR) for incident diabetes compared with age- and sex-matched comparison cohorts without any known rheumatic conditions, after adjusting for body mass index, smoking, alcohol, comorbidities, and glucocorticoids use.
Results: Diabetes developed in 179 of 4,196 individuals with PsA (50% female, mean age 49 years, mean BMI 27.6), in 2,202 of 59,281 persons with psoriasis (51% female, mean age 49 years, mean BMI 26.7), and in 383 of 11,158 individuals with RA (68% female, mean age 58 years, mean BMI 26.8). Age- and sex-matched HRs for diabetes were 1.72 (1.46 – 2.02) in PsA, 1.39 (1.32 – 1.45) in psoriasis, and 1.12 (1.01 – 1.25) in RA relative to the comparison cohorts. After adjustment for BMI, smoking, and alcohol use, these HRs were attenuated substantially (1.43, 1.24, and 1.00, respectively). With further adjustment for glucocorticoid use and comorbidity index, the HRs were 1.33 (1.09 – 1.61) in PsA, 1.21 (1.15 – 1.27) in psoriasis, and 0.94 (0.84 – 1.06) in RA.
Conclusion: This large general population study suggests that the overall risk of diabetes is increased in PsA, which can be substantially explained by increased adiposity, lifestyle factors, and other covariates. In contrast, risk of diabetes among patients with RA is significantly elevated only due to increased BMI and smoking. Overall, these findings suggest that diabetes risk should not be ascribed only to the presence of inflammatory disease. Important opportunities exist for future interventions directed at weight loss and smoking cessation to reduce risk of diabetes in these populations, and to determine how psoriatic disease contributes to the risk of developing diabetes.
Disclosure:
M. Dubreuil,
None;
Y. H. Rho,
None;
A. Man,
None;
Y. Zhu,
None;
Y. Zhang,
None;
T. Love,
None;
A. Ogdie,
None;
J. Gelfand,
Amgen,
5,
Abbott Immunology Pharmaceuticals,
5,
Centocor, Inc.,
5,
Celgene,
5,
Novartis Pharmaceutical Corporation,
5,
Pfizer Inc,
5,
Amgen,
2,
Abbott Immunology Pharmaceuticals,
2,
Pfizer Inc,
2,
Novartis Pharmaceutical Corporation,
2,
Genentech and Biogen IDEC Inc.,
2;
H. Choi,
None.
« Back to 2012 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-risk-of-diabetes-in-psoriatic-arthritis-and-rheumatoid-arthritis/