Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Thrombosis is one of the most frequent manifestations in patients with systemic lupus erythematosus (SLE). Although antiphospholipid antibodies (aPL) are well recognized risk factors for thrombosis in SLE, few studies have addressed the potential effect of additional factors in the development or in the prevention of thrombosis in those patients.
Objective: To identify risk and protective factors for developing thrombosis in SLE with or without aPL.
Methods: One hundred fifty two newly diagnosed consecutive patients with SLE without history of thrombotic events were recruited at Hokkaido University Hospital from April, 1997 to February, 2014. All patients, 138 woman and 14 men, fulfilled the 1997 American College of Rheumatology revised criteria for SLE. Seventy-eight patients (51.3%) had aPL. The development of thrombosis and death caused by thrombosis were defined as the study endpoint.
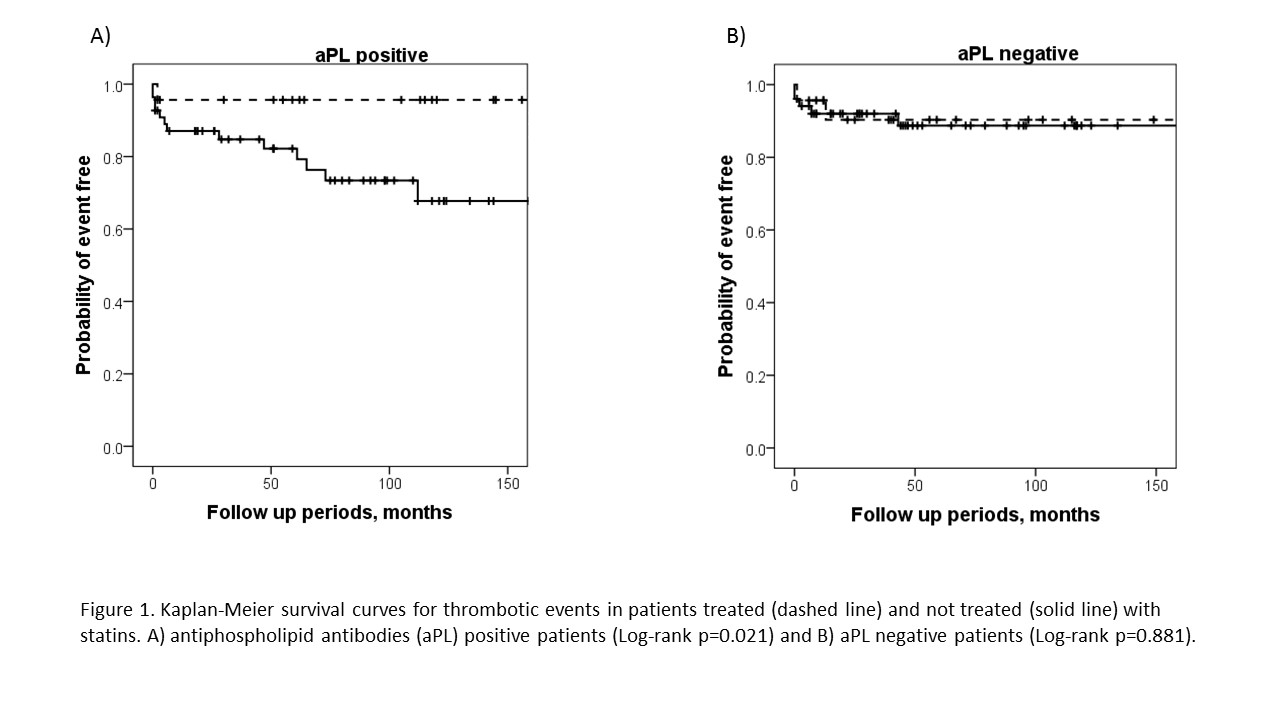
Results: The median follow-up period in all patients was 58 months (IQR 20-115 months). In 78 patients with aPL, the median follow-up period was 69 months (IQR 27-118 months). Fifteen patients with aPL (19.2%) developed thrombosis during the follow-up period. Cerebral infarction (CI) was observed in 6 patients, pulmonary embolism (PE) in 5 and deep vein thrombosis (DVT) in 6. Multivariate analysis with Cox’s proportional hazards model showed that older age at SLE onset and anticardiolipin antibodies (aCL)-IgG positivity, (HR 1.80 for every ten age, 95%C.I. 1.11-2.94) and (HR 6.87, 95%C.I. 1.74-27.1), respectively, are statistically significant risk factor for thrombosis. Statin therapy appears as a statistically significant protective factor against thrombosis (HR 0.12, 95%C.I. 0.01-0.97) (Figure 1.). Disease activity, anti-thrombotic drug therapy and classical risk factors for atherosclerosis were not related to thrombosis. On the other hand, in 74 patients without aPL (median follow-up period 46 months, IQR 15-110 months), 7 patients (9.5%) developed thrombosis. CI was observed in 4 patients, intestinal infarction in 1, PE in 1 and DVT in 1. With Cox’s proportional hazards model, older age at SLE onset represents a statistically significant risk for thrombosis (HR 2.73 for every ten age, 95%C.I. 1.17-6.37).
Conclusion: This study suggests that, in aPL positive patients, the late disease onset and the presence of aCL-IgG represent additional risk factors for thrombosis. Statin treatment appeared as a thrombotic protective factor.
Disclosure:
T. Watanabe,
None;
K. Oku,
None;
O. Amengual,
None;
E. Sugawara,
None;
R. Hisada,
None;
K. Ohmura,
None;
T. Fukui,
None;
S. Shimamura,
None;
I. Nakagawa,
None;
A. Noguchi,
None;
H. Shida,
None;
M. Kono,
None;
Y. Shimizu,
None;
T. Kurita,
None;
T. Bohgaki,
None;
T. Horita,
None;
S. Yasuda,
None;
T. Atsumi,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-protective-effects-of-statins-for-thrombosis-in-patients-with-systemic-lupus-erythematosus-positive-for-antiphospholipid-antibodies/