Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Psoriatic arthritis (PsA) is a chronic inflammatory disease with a heterogeneous presentation that is associated with impaired quality of life, joint damage, and limited ability to work.1–3 Diagnosis of PsA is often challenging and may require close collaboration between dermatologists and rheumatologists. Reliance on laboratory and/or radiographic tests to diagnose PsA varies among rheumatologists. The PREPARE trial (NCT01147874) was conducted to estimate PsA prevalence as determined by rheumatologists’ evaluation of psoriasis patients presenting to dermatologists’ offices. The objective of the secondary analysis presented here was to estimate the prevalence of PsA in psoriasis patients based on clinical assessment by rheumatologists using medical history and physical examination before and after review of supplemental laboratory and radiographic tests.
Methods: Unselected, consecutive psoriasis patients, ≥18 years of age, were initially assessed for plaque psoriasis by dermatologists at 34 dermatology centers in 7 European and North American countries. After psoriasis was confirmed, patients were evaluated for PsA by rheumatologists based on medical history and physical examination alone. Rheumatologists reassessed their diagnoses after receiving laboratory test results (eg, C-reactive protein, erythrocyte sedimentation rate, or rheumatoid factor). In a patient subgroup undergoing radiographic evaluation of hands and feet, rheumatologists conducted a 2nd reassessment after x-rays were provided.
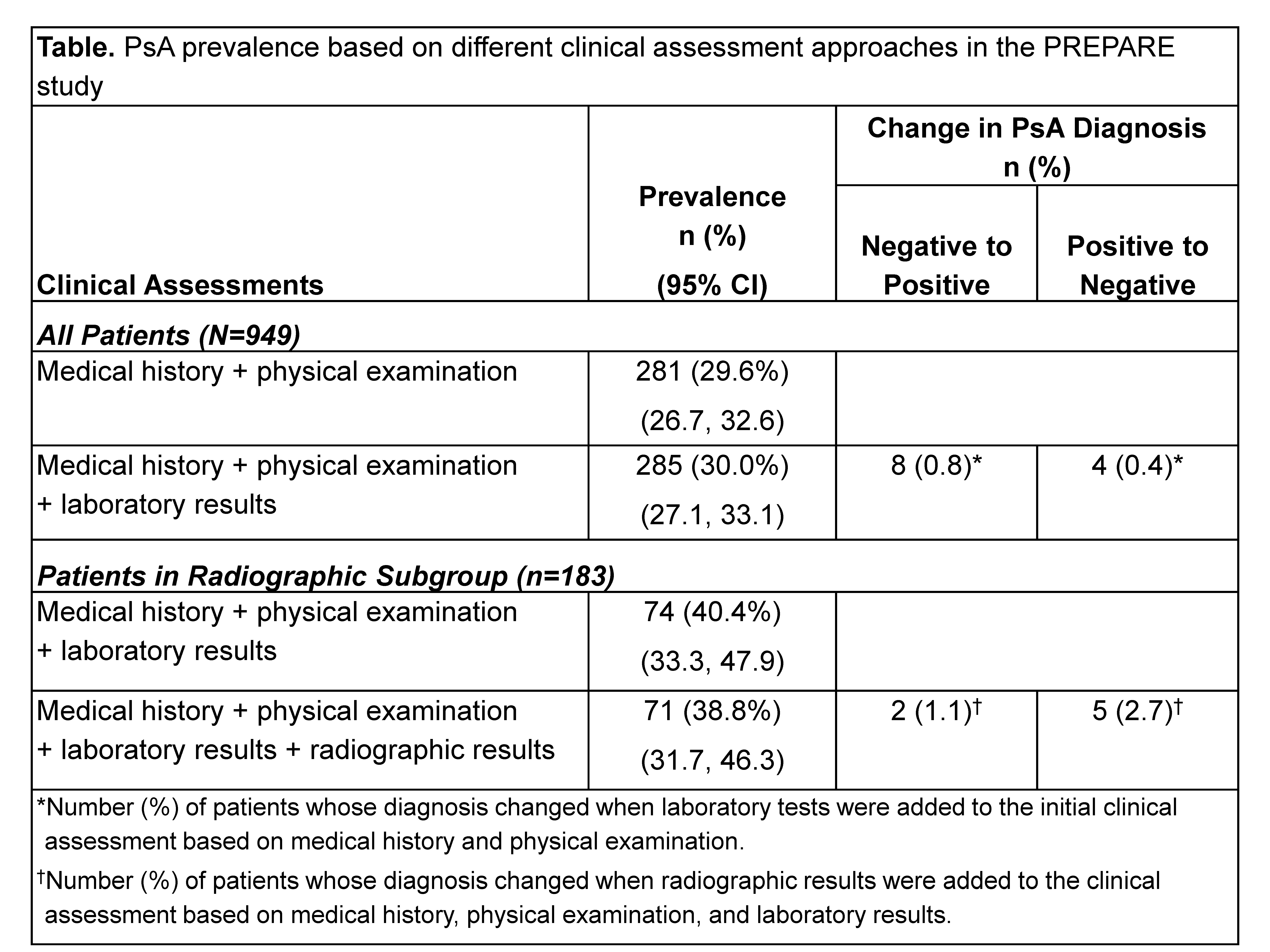
Results: In 949 psoriasis patients who were subsequently evaluated with the inclusion of laboratory tests, 281 (29.6%) were initially diagnosed with PsA based on medical history and physical examination alone (table). In comparison, 285 (30.0%) received clinical PsA diagnoses from rheumatologists based on medical history, physical examination, and laboratory results. In 183 psoriasis patients in the radiographic subgroup, 74 (40.4%) received a PsA diagnosis based on medical history, physical examination, and laboratory results, whereas 71 (38.8%) received this diagnosis based on medical history, physical examination, laboratory results, and radiographic findings.
Conclusion: In this large, multinational prevalence study, approximately one-third of psoriasis patients had PsA based on rheumatologists’ clinical assessment. This analysis confirms the ability of rheumatologists to diagnosis PsA based on medical history and physical examination alone. However, laboratory and radiographic results may assist in excluding and/or confirming the diagnosis in some patients.
References: 1. Husted JA, et al. Arthritis Rheum 2001; 45: 151-8. 2. Rahman P, et al. J Rheumatol 2001; 28: 1041-4. 3. Tillett W, et al. Rheumatology (Oxford, England) 2012; 51: 275-83.
Disclosure:
D. D. Gladman,
Abbott Laboratories, Amgen, BMS, Janssen, Pfizer,
2;
P. J. Mease,
Abbott, Amgen, Biogen Idec, BMS, Celgene, Crescendo, Forest, Genentech, Janssen, Lilly, Merck, Novartis, Pfizer, UCB,
2,
Abbott, Amgen, Biogen Idec, BMS, Celgene, Crescendo, Forest, Genentech, Janssen, Lilly, Merck, Novartis, Pfizer, UCB,
5,
Abbott, Amgen, Biogen Idec, BMS, Crescendo, Forest, Genentech, Janssen, Lilly, Pfizer, UCB,
8;
R. Y. Faraawi,
Pfizer, Roche, Janssen, Merck,
5,
Pfizer, Roche, Janssen, Merck,
8;
E. Bananis,
Pfizer Inc,
1,
Pfizer Inc,
3;
A. S. Koenig,
Pfizer Inc,
3;
R. Northington,
Pfizer Inc,
1,
Pfizer Inc,
5;
J. Fuiman,
Pfizer Inc,
1,
Pfizer Inc,
3;
D. Alvarez,
Pfizer Inc,
3.
« Back to 2012 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-prevalence-of-psoriatic-arthritis-based-on-rheumatologists-clinical-assessment-before-and-after-laboratory-and-radiographic-tests-in-psoriasis-patients-in-europeannorth-american-dermatol/