Session Information
Date: Monday, October 27, 2025
Title: Abstracts: ARP I: Multidimensional Influences on Health in SLE (1686–1691)
Session Type: Abstract Session
Session Time: 3:00PM-3:15PM
Background/Purpose: Depression is reported to be common in SLE, but little is known about depressive symptoms among older adults with SLE. While the burden of comorbid conditions and the cumulative effects of SLE may be heightened in this group,1 odds of depression are higher in younger age groups in the general population.2 Screening for depression appears to be uncommon in rheumatology settings. We compared depressive symptom levels and the self-reported awareness of depression among older adults with SLE to those with RA and OA.
Methods: Data were from FORWARD, The National Databank for Rheumatic Diseases, a longitudinal observational cohort. Data are collected semiannually. Individuals with diagnosed SLE, rheumatoid arthritis (RA), and osteoarthritis (OA) were included in analyses; those with concurrent fibromyalgia were excluded. Depressive symptoms were assessed with the Patient Heath Questionnaire (PHQ)-8 over 4 survey periods. PHQ-8 scores were classified as ≥mild (≥5) or ≥moderate (≥10) levels of depressive symptoms. Persistent depression was defined as mild/moderate symptoms at ≥2 time points. Generalized estimating equation (GEE) regression analyses (unadjusted and adjusted for age, sex, education, disease duration, physical function, and pain) compared scores among the 3 groups. The proportion of individuals with notable levels of depressive symptoms who did not self-report with depression was examined.
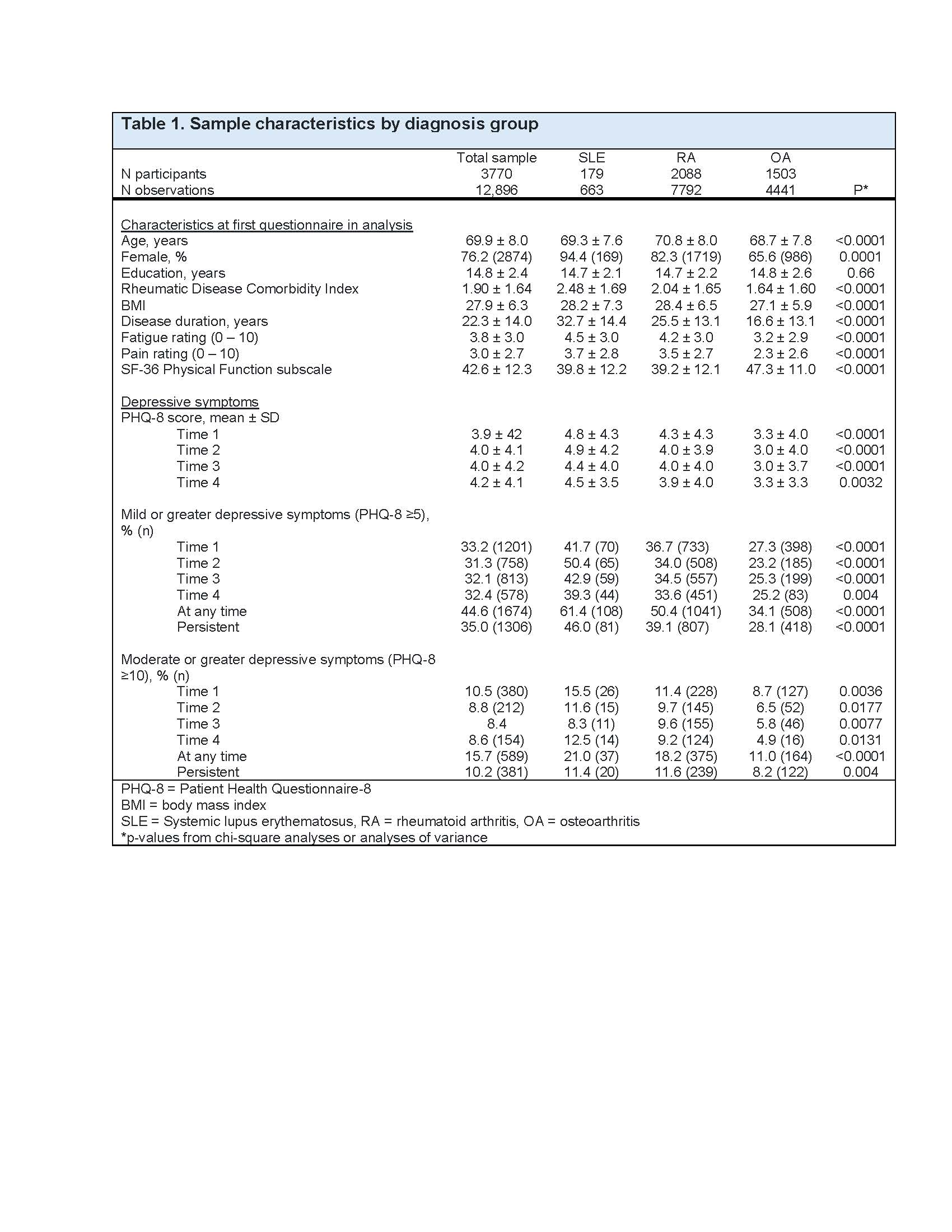
Results: Data from 3770 participants (12,896 observations) were included (SLE n=179, obs=663; RA n=2088, obs=7792; OA n=1503, obs=4441). Mean age was 69±8 years (Table 1). Across years, with only one exception, older adults with SLE had higher PHQ-8 scores and higher frequencies of scores ≥5, and ≥10. Any occurrence of PHQ-8 scores ≥10 was seen in 21.0%, 18.2%, and 11.0% of those with SLE, RA, and OA, respectively. Persistent PHQ-8 scores ≥10 were found in 11.4%, 11.6%, and 8.2% of those with SLE, RA, and OA. GEE analyses (unadjusted and adjusted) showed significantly higher PHQ-8 scores and significantly higher prevalence of mild depressive symptoms in SLE compared to RA and OA (Table 2). Prevalence of moderate symptoms were significantly higher in SLE compared to OA in unadjusted analyses, but differences were attenuated after adjustment. In each year, at least 2/3 of those with ≥mild and about half of those with ≥moderate depressive symptoms did not self-report having depression (Table 3).
Conclusion: Older adults with SLE appear to carry a greater burden of depressive symptoms than individuals of similar age with RA or OA, and large portions of individuals seem to be unaware of having depressive symptoms. Given this lack of awareness, the reported low levels of screening, and the significant impact of depression on health and well-being, results support greater attention to mental health in clinical encounters, particularly among older adults with SLE.
1 Leiber S et al. J Rheumatol 2025; 52:145-150.
2 Hasin D et al. JAMA Psychiatry 2018; 75:336-346
To cite this abstract in AMA style:
Katz P, Pedro S, Michaud K. The Prevalence of Depressive Symptoms and Persistent Depression among Older Adults with Systemic Lupus Erythematosus (SLE) [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/the-prevalence-of-depressive-symptoms-and-persistent-depression-among-older-adults-with-systemic-lupus-erythematosus-sle/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-prevalence-of-depressive-symptoms-and-persistent-depression-among-older-adults-with-systemic-lupus-erythematosus-sle/

.jpg)
.jpg)