Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: An administration of tocilizumab (TCZ) rapidly suppresses inflammatory markers such as CRP and ESR, which makes the diagnosis of infection difficult. There is a real need to establish the surrogate marker of infectious disease and to find how to reduce the infection risk. / To validate the specificity of CD64 on polymorphonuclear neutrophils (CD64) and procalcitonin (PCT) levels as parameters for serious infection (SI) and deterrence effect of infectious disease risk management (IDRM) in RA patients with TCZ.
Methods: Forty-nine RA patients with were enrolled from 4 universities and affiliated clinics (Table). They were required to comply with IDRM policy during observation period. CD64 and PCT were measured at week 0, 4, 8 and the occurrence of infectious disease. Primary endpoint was occurrence frequency of SI (OFSI) and rate of increase in CD64 and PCT. Secondary endpoint was admission due to infection, the dose of concomitant medicines, CDAI and persistence rate of TCZ.
Table Baseline characteristics of RA subjects at cohort entry
|
Cases (Male/Female) |
49 (5/44) |
|
Age (yr) |
57.9 |
|
Weight |
54.3 |
|
Disease duration (yr) |
8.0 |
|
Steinblocker’s Stage (1/2/3/4) |
18.8/35.4/22.9/22.9 |
|
Steinblocker’s Class (1/2/3/4) |
22.9/62.5/14.6/0 |
|
Smoking |
14.3% |
|
Steroid use |
59.2% |
|
Daily dose(mg as equivalent with prednisolone) |
5.8 |
|
Methotrexate use |
64.0% |
|
Weekly dose (mg) |
8.7 |
Results: CD64 was 1477.3±199 and 1456.1±96.7 before and after TCZ administration, respectively. There was no significant difference of CD64 and PCT at baseline between patients with infectious disease and without infectious disease (1104.8±228.3 vs. 1501.4±191.5). Although the increase of CD64 was found in patients with infectious disease at week 8 compared with patients having no infectious disease, there were no significant difference between two groups (2091.2±934.9 vs. 1405.2±157.9). CRP was not as sensitive as CD64, which increased more than 2,000 when infection was complicated in some, but not all cases.

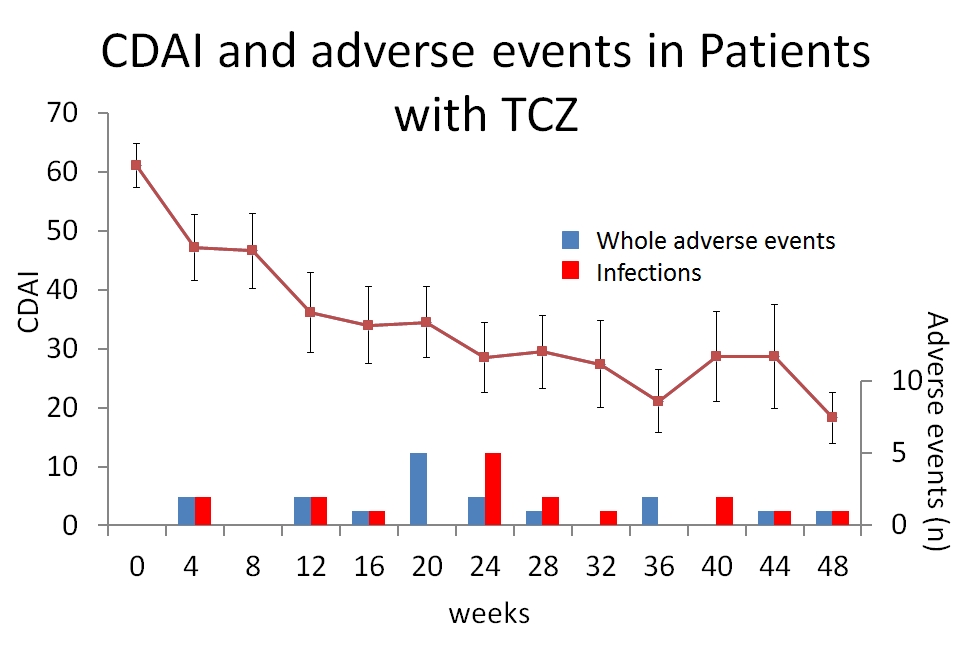 Neither pneumonia nor cellulitis occurred in 17 events of infection and 3 events of SI. CDAI was changed from 61.1±3.7 to 18.3±4.4 (Figure). The dose of CS was reduced by 41.8%. Persistence rate of TCZ was 69.4% at 48 weeks (Figure).
Neither pneumonia nor cellulitis occurred in 17 events of infection and 3 events of SI. CDAI was changed from 61.1±3.7 to 18.3±4.4 (Figure). The dose of CS was reduced by 41.8%. Persistence rate of TCZ was 69.4% at 48 weeks (Figure).
Conclusion: The present study showed that CD64 more sensitively moved than CRP at the complication with infection, suggesting that CD64 was a promising surrogate marker to detect infectious events in patients treated with TCZ. In spite of higher frequency of concomitant lung disease, the incidence of respiratory infection and OFSI were lower in our study than PMS, indicating that IDRM could contribute to reduction of OFSI especially in respiratory infection.
Disclosure:
A. Ihata,
None;
H. Hagiyama,
None;
S. Nagaoka,
None;
J. Obata,
None;
K. Miyachi,
None;
H. Yamada,
None;
S. Hirohata,
None;
N. Koido,
None;
M. Yamasaki,
None;
K. Miyagi,
None;
S. Ohno,
None;
D. Kishimoto,
None;
R. Watanabe,
None;
T. Uehara,
None;
K. Takase,
None;
M. Hama,
None;
R. Yoshimi,
None;
A. Ueda,
None;
M. Takeno,
None;
Y. Ishigatsubo,
None.
« Back to 2012 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-predictive-value-of-cd64-counts-for-infectious-disease-in-patients-treated-with-tocilizumab-on-the-infectious-disease-risk-management-cohort-act4u-study/
