Session Information
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: There is limited information about the constellation of musculoskeletal symptoms experienced by patients with early psoriatic arthritis (PsA). This study aims to describe the pattern of musculoskeletal symptoms and their correlation with clinical and sonographic findings among psoriasis patients with suspected PsA.
Methods: The study evaluated patients with psoriasis and musculoskeletal complaints who did not have a prior diagnosis of PsA. These patients were evaluated in a rapid access clinic that included a central triage system using the following modalities: 1) screening questionnaires that included homunculus where patients marked the location of the affected joints, 2) assessment by an advanced practice physiotherapist, 3) musculoskeletal ultrasound (MSK-US) of joints and entheses. In addition, patients completed questionnaires about the nature and duration of their musculoskeletal symptoms, physical function and quality of life. All patients were then assessed by a rheumatologist who classified each patient to: “PsA”, “Not PsA”, or “Possibly PsA”. Agreement between modalities was assessed using Kappa statistics.
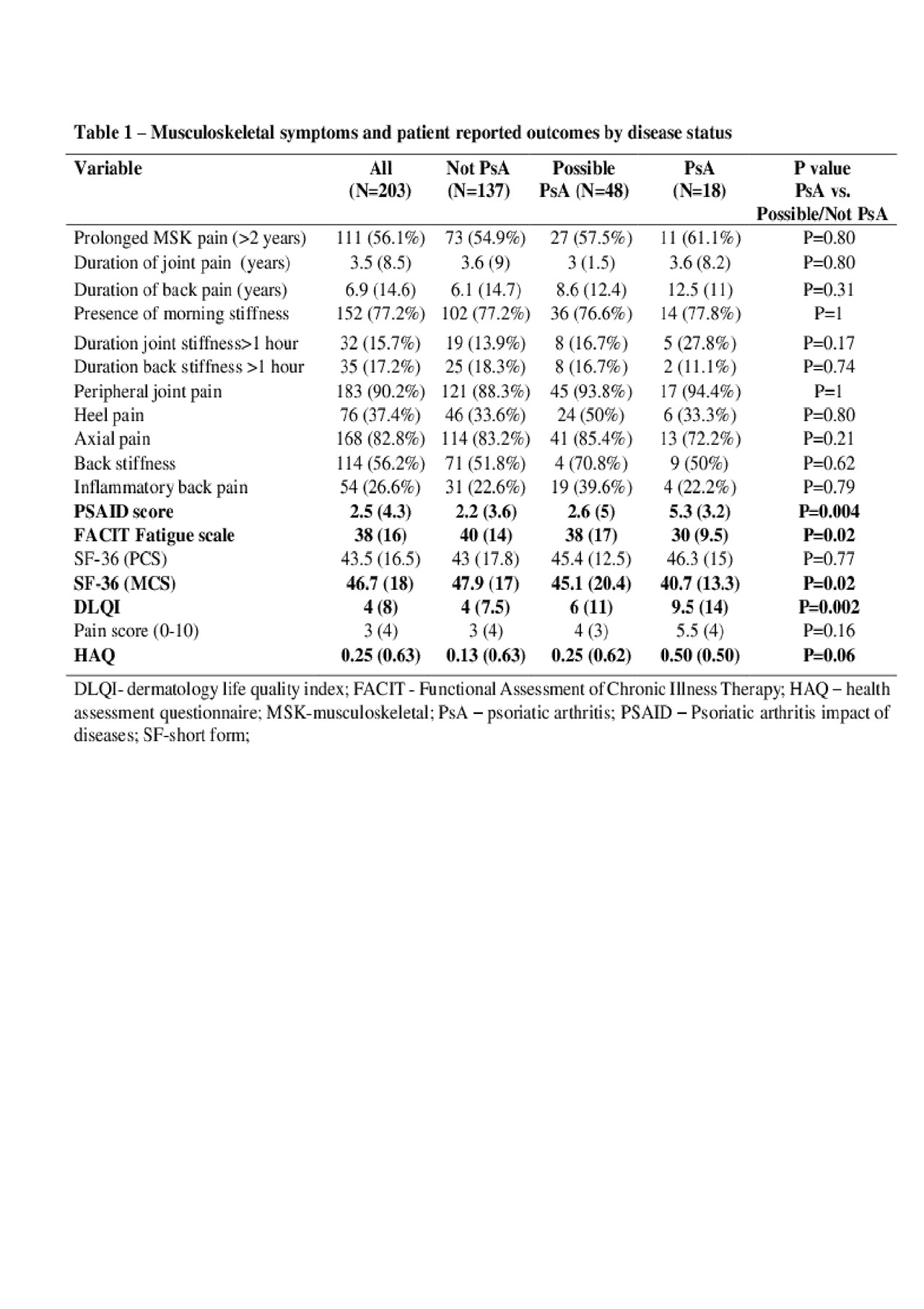
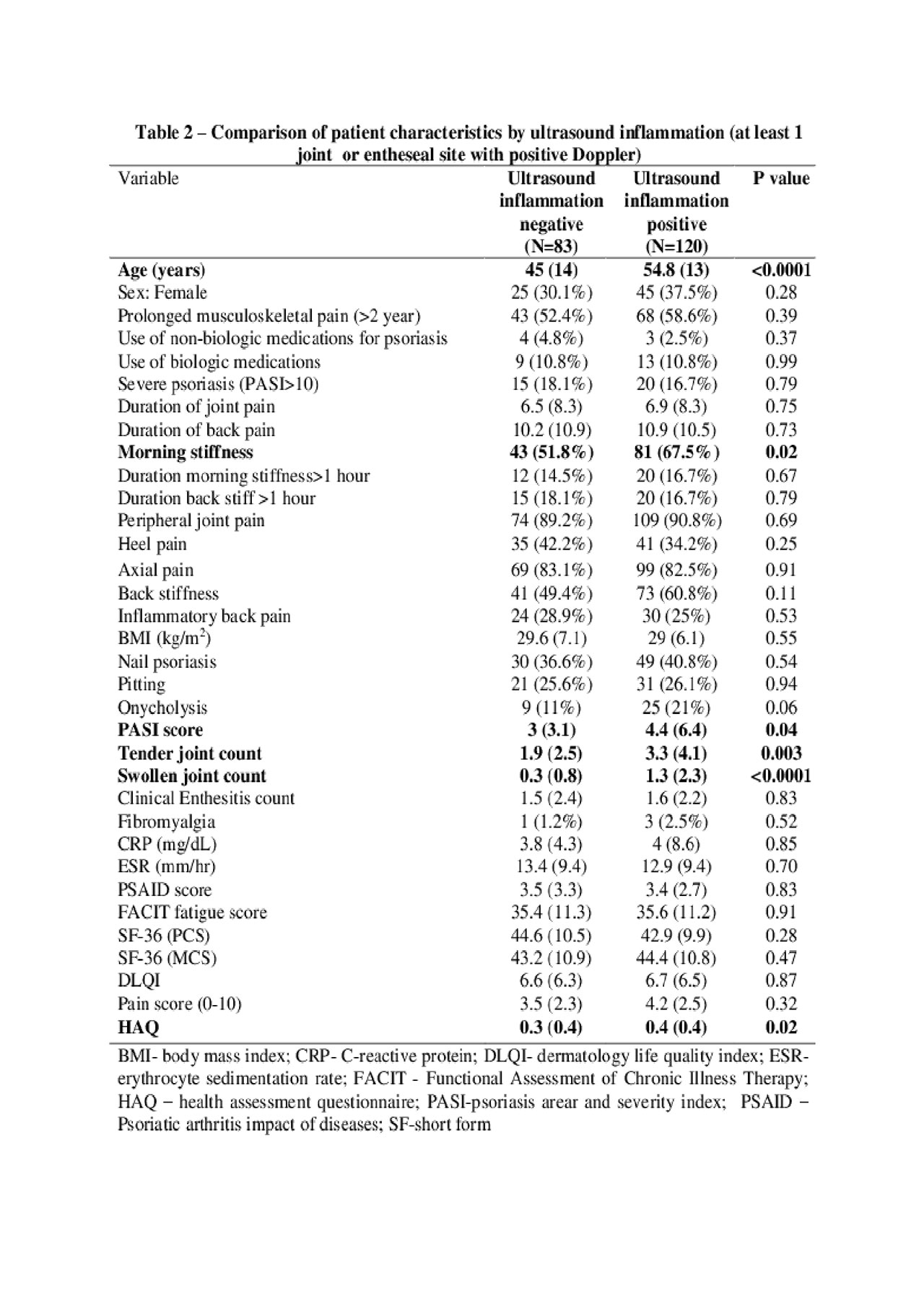
Results: 203 patients with psoriasis and musculoskeletal symptoms were enrolled in the study. 18 (8.8%) and 48 (23.6%) were classified as “PsA and “possible PsA”, respectively. There was no difference between the two groups in the presence, distribution and duration of musculoskeletal pain (Table 1). Patients with PsA had higher intensity of musculoskeletal and skin-related symptoms (DLQI) and worse scores in domains such as physical function (HAQ), quality of life (PSAID) and fatigue (FACIT). Patients who were classified as “PsA” were more likely to use systemic medications for psoriasis (< 0.05), have severe psoriasis (p=0.02) and nail lesions (p=0.02) and have synovitis/enthesitis by MSK-US (p=0.01). Patients with positive MSK-US inflammation were older (p< 0.001), reported more joint stiffness (p=0.02) and physical dysfunction (by HAQ, p=0.02, Table 2), irrespective of the clinical diagnosis. Analysis of agreement between modalities revealed the strongest agreement between the rheumatologist and physiotherapist (k=0.28, Table 3). The lowest levels of agreement were found between ultrasound and patient (k=0.08) and physiotherapist and ultrasound (k=0.08).
Conclusion: The intensity, rather than the type, duration or distribution of musculoskeletal symptoms, is associated with psoriatic arthritis among patients with psoriasis. The correlation between musculoskeletal symptoms, patient reported outcomes and sonographic findings is poor in patients with suspected PsA. MSK-US provides additional information to the clinical assessment and aid in diagnosing PsA patients at earlier stages.
To cite this abstract in AMA style:
Sarabia S, Farrer C, Yeung J, Cook R, Lee K, Jerome D, Eder L. The Pattern of Musculoskeletal Complaints in Patients with Suspected Psoriatic Arthritis and Their Correlation with Physical Examination and Ultrasound [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-pattern-of-musculoskeletal-complaints-in-patients-with-suspected-psoriatic-arthritis-and-their-correlation-with-physical-examination-and-ultrasound/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-pattern-of-musculoskeletal-complaints-in-patients-with-suspected-psoriatic-arthritis-and-their-correlation-with-physical-examination-and-ultrasound/