Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Psoriatic arthritis (PsA) is a heterogenous inflammatory disease affecting skin, joints, and other domains. While psychiatric diseases (i.e., depression and anxiety) are known comorbidities, little is known about their impact on disease severity and patient reported outcomes (PROs). The objective of this study was to characterize the prevalence of psychiatric comorbidities in an academic combined psoriasis-psoriatic arthritis center and determine their impact on PsA clinical and patient derived outcomes.
Methods: Consecutive adult patients meeting CASPAR criteria for PsA (n=436) were prospectively recruited at the NYU Psoriatic Arthritis Center. All data was collected from clinical visits utilizing a standardized EPIC template. Depression was defined by established diagnosis and/or use of anti-depressant medications. Objective measures of disease severity included swollen and tender joint counts (SJC/TJC) and PROs including RAPID3 scores. Data was analyzed using statistical software R.
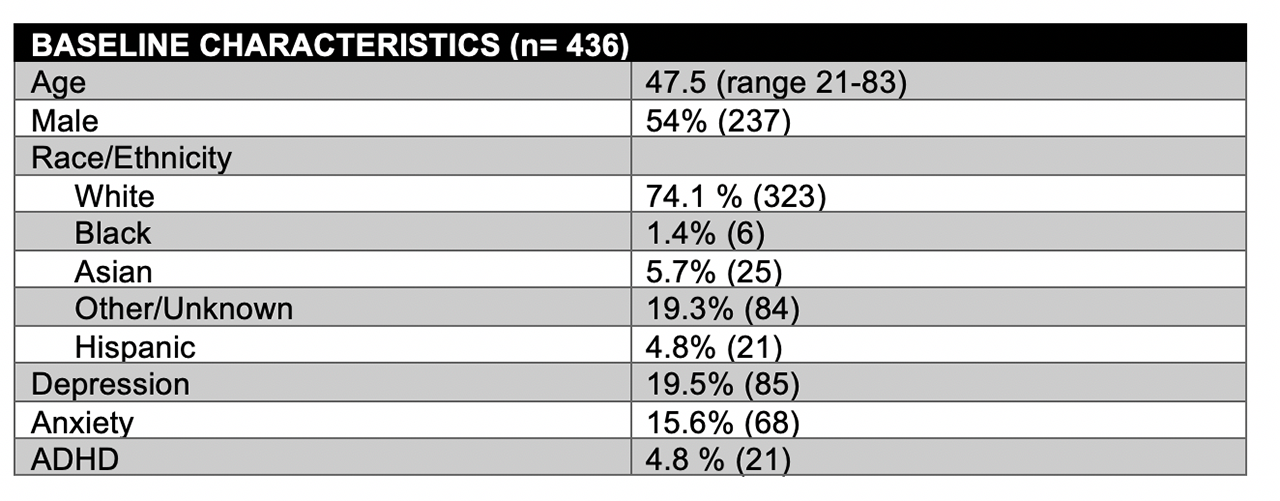
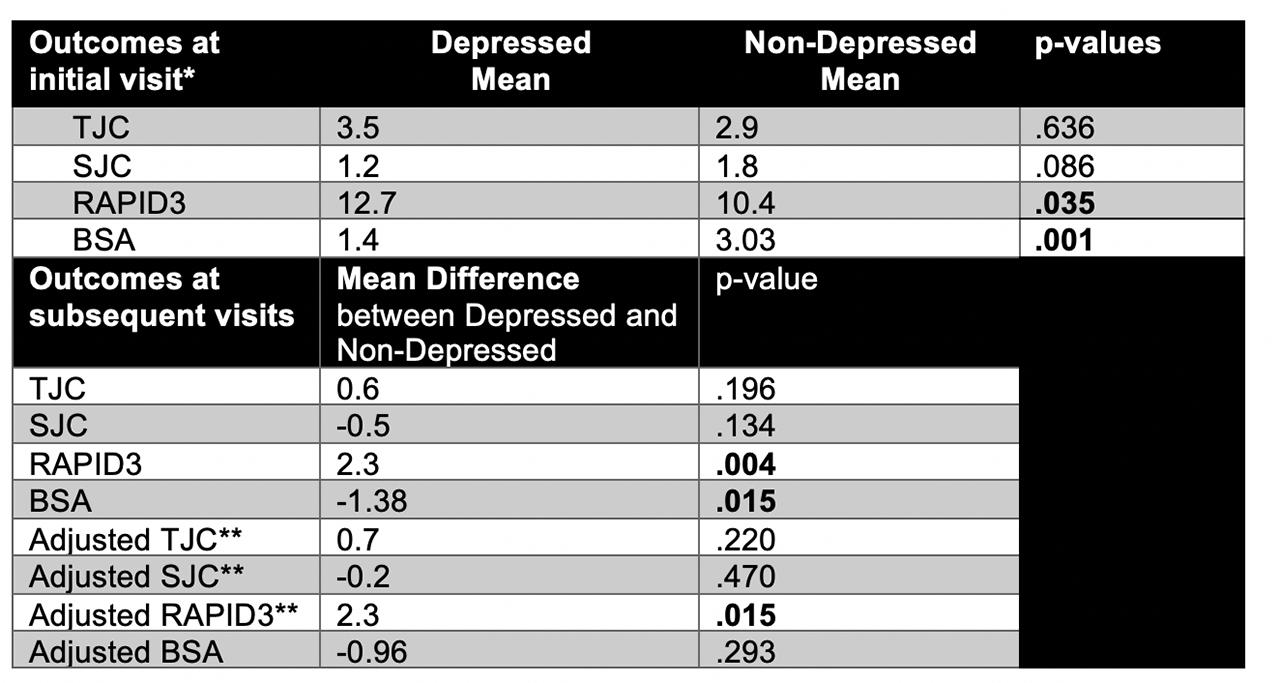
Results: Our cohort was comprised of 436 patients: 54% male, mean age of 47 years, and mostly Caucasians (74.1%). Within our population, 19.5% had depression, 15.6% had anxiety, and 4.8% had ADHD (Table 1). Of those with depression, 71% were on anti-depressive medication. At the initial visit, patients with PsA and depression were more likely to be on medication(s) for PsA (80% vs 65%, p=.01) and had a trend towards higher rates of biologic use (47.5% vs 40.4%, p=.126). Those with depression had a similar TJC to their non-depressed counterparts, but had a trend towards fewer swollen joints and concomitant higher RAPID3 scores (Table 2). When analyzing repeated outcome measures over subsequent visits, individuals with depression were similarly more likely to have a higher TJC, a lower SJC, and a higher RAPID3 score (although only RAPID3 was found to be statistically significant, p=.004). Importantly, these findings persisted when analyzing participants that were matched with propensity scores to adjust for age, sex, comorbidities, and medication use. In addition to joint activity, psoriasis activity measured by body surface area (BSA) was lower in those who were depressed (1.4% vs 3.03%, p=.001) and these differences were maintained over subsequent visits.
Conclusion: Our results expand on prior reports of significantly elevated rates of depression in PsA. Notably, individuals with depression were more likely to be on medication(s) for their PsA, had fewer swollen joints, and a lower BSA but, paradoxically reported higher RAPID3 scores. This discrepancy is likely a manifestation of how depression could affect the way patients experience their PsA despite apparent improvement in skin and joint symptoms. Depression should, therefore, be considered a critical comorbidity when addressing PsA care in routine visits. Further work is needed to understand whether modulation of psychiatric comorbidities can lead to improved PsA outcomes.
*Outcomes at the initial visit were analyzed using t-test. Repeated measures were analyzed with Satterthwaite’s approximations for the t test within mixed effects linear model with gaussian errors. P-values of equal to or less than .05 were considered significant.
** Adjusted using matching by propensity score that included age, sex, multiple comorbidities, and medication use.
To cite this abstract in AMA style:
Haberman R, Adhikari S, Ramirez D, Lydon E, Attur M, Neimann A, Reddy S, Troxel A, Scher J. The Paradoxical Effect of Depression on Psoriatic Arthritis Outcomes in a Combined Psoriasis-Psoriatic Arthritis Center [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-paradoxical-effect-of-depression-on-psoriatic-arthritis-outcomes-in-a-combined-psoriasis-psoriatic-arthritis-center/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-paradoxical-effect-of-depression-on-psoriatic-arthritis-outcomes-in-a-combined-psoriasis-psoriatic-arthritis-center/