Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Pulmonary arterial hypertension (PAH) is a major complication in systemic sclerosis (SSc) and is characterized by abnormalities in vascular pathways. In murine models of PAH increased lymphangiogensis has been shown in lung tissue by elevated vascular endothelial growth factor receptor 3 (VEGFR-3) expression, which is a known lymphatic marker. The ligand acting through VEGFR-3 is vascular endothelial growth factor C (VEGF-C), a major growth factor in the lymphatic vessels under physiological conditions. We have shown that VEGF-C is downregulated in SSc patients and aim to assess the characteristics of VEGF-C and its receptor VEGFR-3 in SSc patients, and investigate the VEGF-C/VEGFR-3 axis in SSc-PAH.
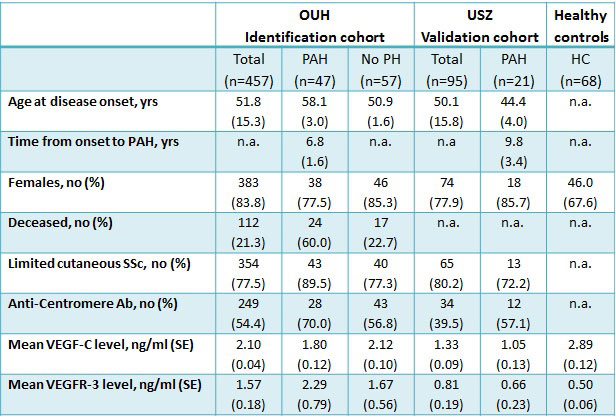
Methods: Sera samples from the SSc cohorts at Oslo University Hospital (n=457, identification cohort) and Zurich University Hospital (n=95, validation cohort), as well as age and gender matched healthy controls (n=68) were included in the study, and analyzed for soluble VEGF-C and VEGFR-3 levels by Luminex kits from Millipore. SSc patients with clinically suspect PH were referred to right heart catheterization (RHC). Mean pulmonary arterial pressure (mPAP) ≥21 mmHg in the absence of significant interstitial lung disease and a PVR ≥ 3 Wood Units (WU) was defined as PAH, whereas PVR < 3 WU was defined as early PAH. Descriptive statistics were performed and correlations were calculated by non-parametric Spearman’s rho analysis.
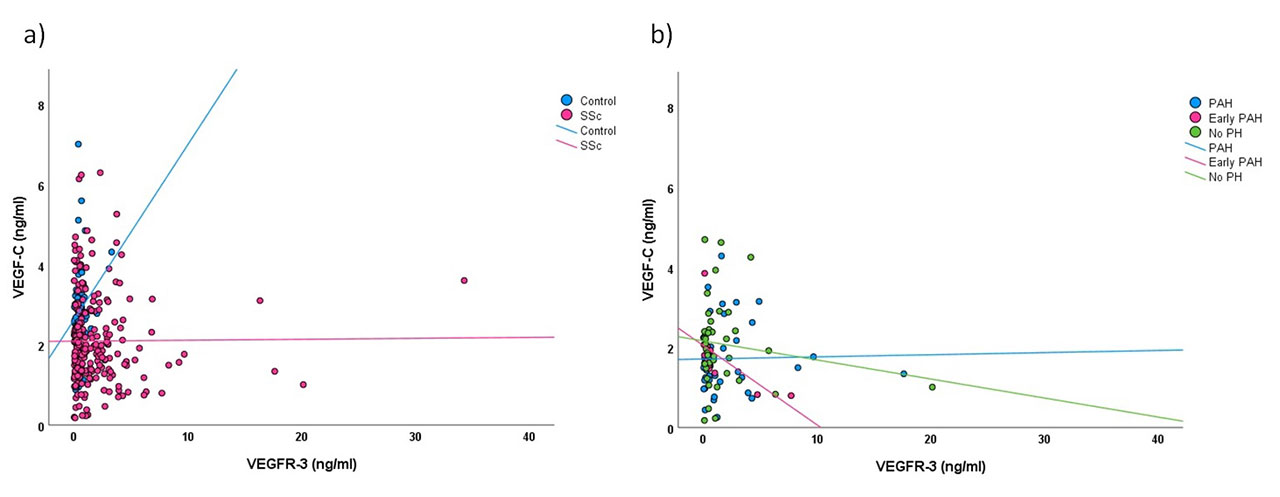
Results: The demographics and clinical data of SSc patients were similar in the Oslo identification and Zurich validation cohorts (Table 1), and were assembled for further analysis. Serum levels of VEGF-C were significantly lower in SSc patients than in healthy controls (2.1±0.04 ng/ml vs. 2.9±0.12 ng/ml, p< 0.001), while serum levels of VEGFR-3 were significantly higher in SSc compared to healthy controls (1.8±0.20 ng/ml vs. 0.5±0.06 ng/ml, p=0.001) in both cohorts. A total of 238 (43.1%) patients were assessed by RHC. Patients with post-capillary (n=51), PH-ILD (n=32) and early PH-ILD (n=6) were excluded, while the remaining 149 RHC verified patients were included in the investigation of VEGF-C and VEGFR-3 serum levels; including 68 patients with PAH, 22 with early PAH and 59 with no PH. Correlation of VEGF-C and VEGFR-3 were weak in SSc patients and healthy controls (r=0.1, p=0.150 vs. r=0.3*, p=0.020), and the difference between the correlation coefficients were not significant (p=0.083). The correlation between VEGF-C and VEGFR-3 in SSc cases having RHC findings of PAH and no PH were also weak (r=0.3*, p=0.034 vs. r=-0.1, p=0.337) with no significant difference between the correlation coefficients (p=0.057). Notably, the correlation in early PAH subjects were strong (-0.8*, p=0.001), and there was a significant difference between the correlation coefficients of early PAH and PAH (p=0.001) and early PAH and no PH groups (p=0.003) (Figure 1).
Conclusion: VEGF-C and its receptor VEGFR-3 is associated with SSc, and the observed skewing of VEGF-C/VEGFR-3 ratios in early and established PAH indicates dysregulation of the VEGF-C/VEGFR-3 axis during development of PAH.
« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-lymphangiogenetic-factor-vegf-c-and-its-receptor-vegfr-3-are-associated-with-pulmonary-arterial-hypertension-in-systemic-sclerosis/