Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Psoriatic arthritis (PsA) is a complex inflammatory musculoskeletal disease associated with psoriasis. This study was conducted to investigate the diagnostic journey to PsA, exploring the duration from symptom onset to diagnosis.
Methods: All reachable PsA patients registered in our clinic (between 2000 and 2024) were included and enrolled in the study survey.
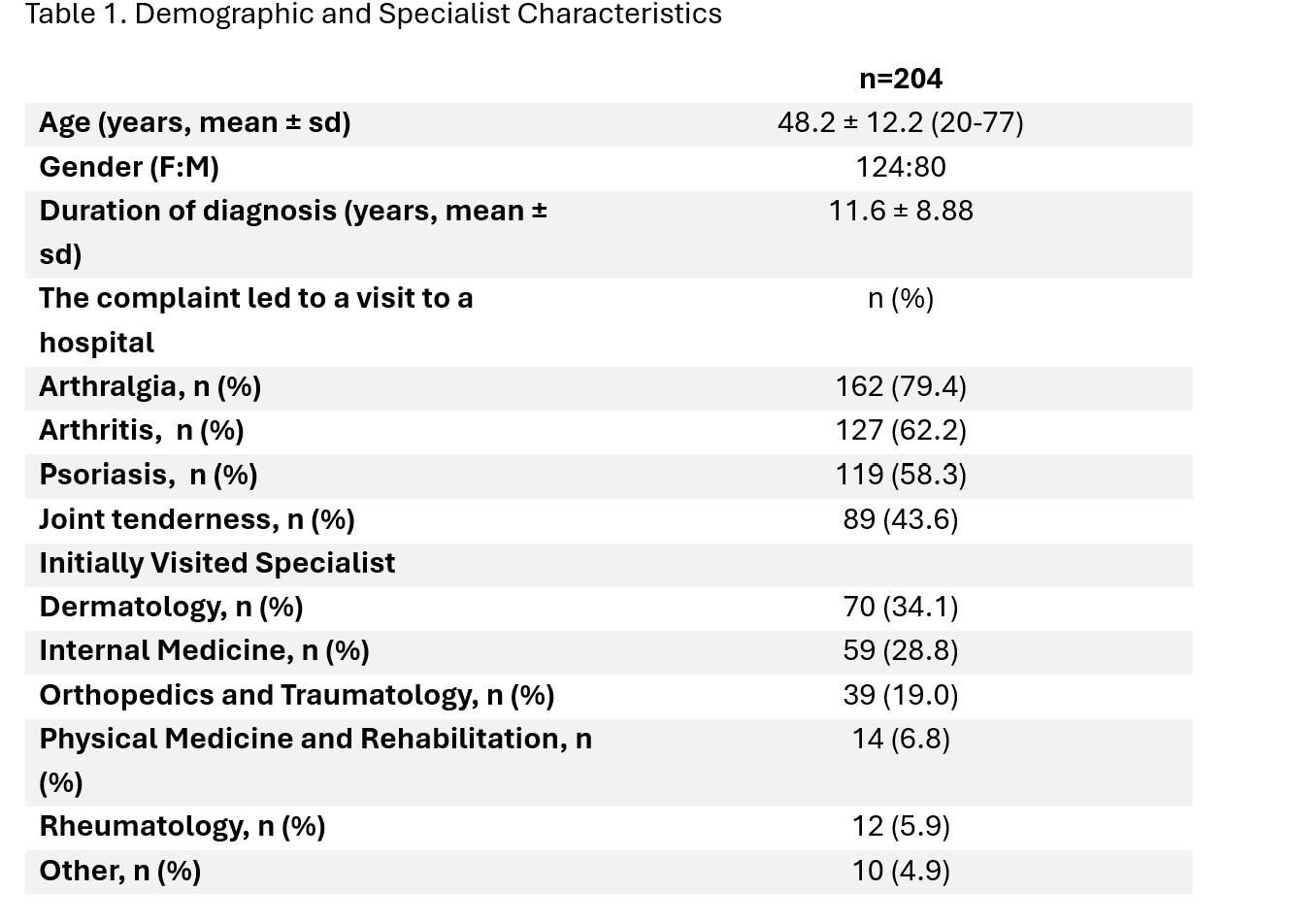
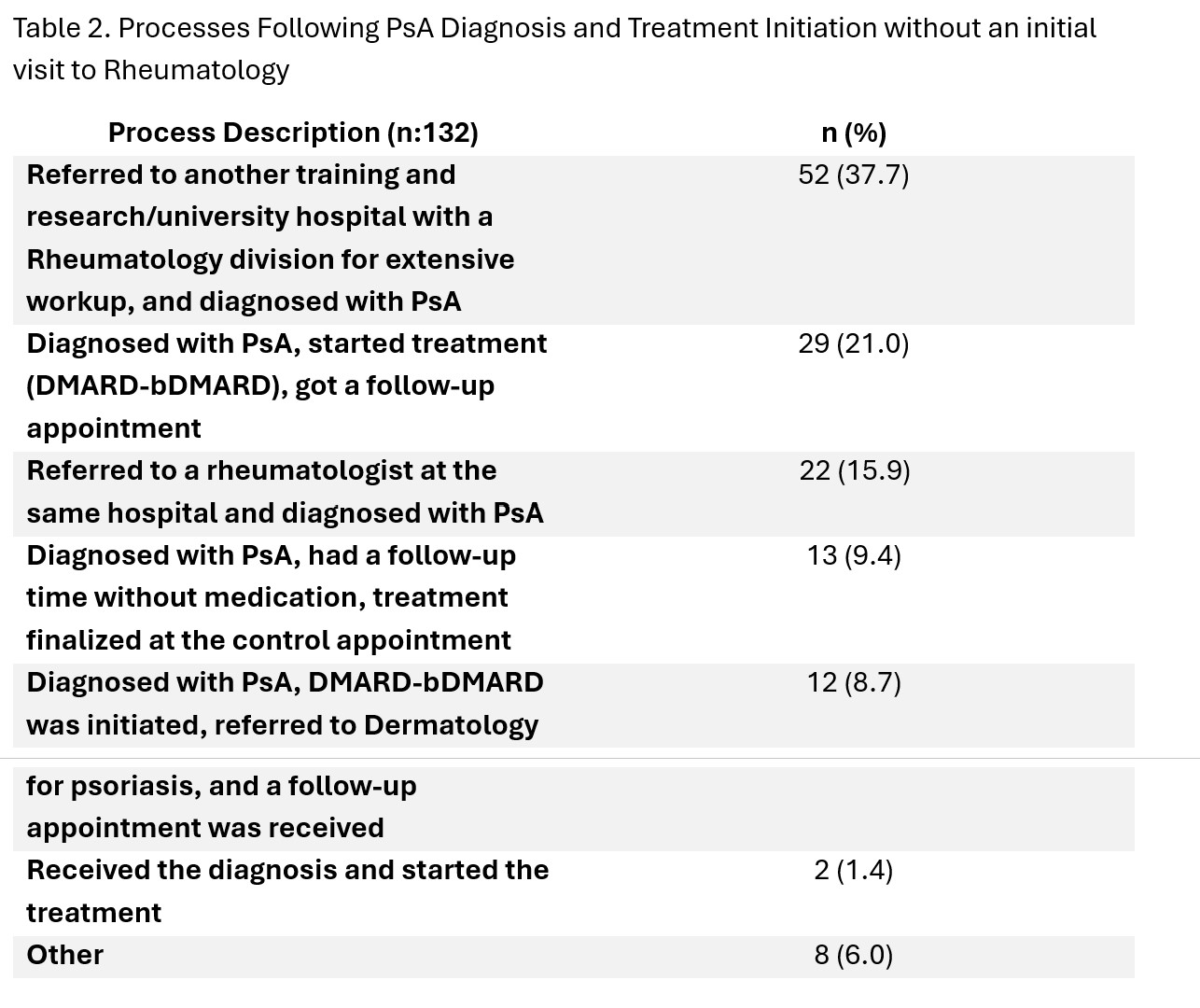
Results: A total of 204 patients, with a mean age of 48.2 ± 12.2 years (range 20-77), were included in the study. The group consisted of 80 males and 124 females. Before receiving their PsA diagnosis, patients initially sought help from dermatology (34.1%), internal medicine (28.8%), and orthopedics (19.0%) (Table 1). Only 11.5% of patients directly visited a rheumatology department. Among patients who did not initially seek help from rheumatology, 37.7% were later referred to a rheumatology department at a training and research hospital or a university hospital for further evaluation, where they received a diagnosis of PsA (Table 2).
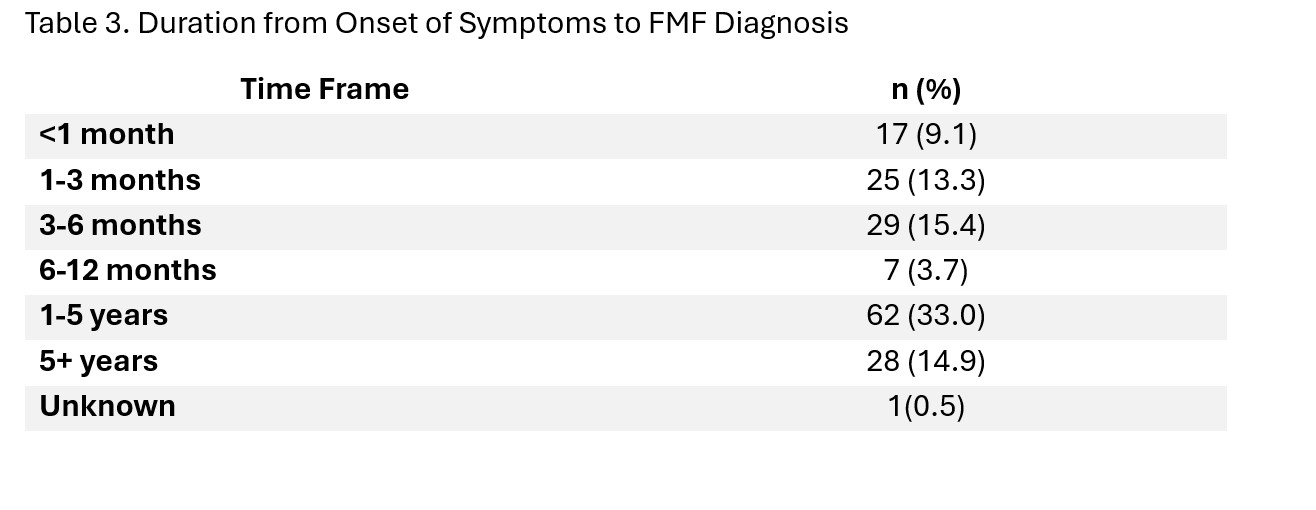
61.4% of the patients who first applied to rheumatology started their treatment after the workups and got their follow-up appointment. 26.5% of patients were applied to more than three specialists until their final diagnosis. 49.7% of them got their diagnosis at a university hospital. From their symptom onset to receiving a diagnosis, 33% of the patients spent around 1-5 years in total (Table 3). 44.6% of the patients continued their follow-up with the doctor who initially diagnosed them.
After the patients were diagnosed, 19.9% of them began their treatment right away. Among the tests conducted for the diagnosis, biopsy, and blood tests took the longest to complete for 50.8% of the patients. Specifically, 7.6% of the patients who underwent biopsy and blood tests reported that the process took about 2 months.
The latest treatment data shows that 59.9% of the patients had to switch to another medication. Patients typically had to wait about 3 months between appointments with the rheumatologist. Only 41.2% of the patients were able to secure their next appointment at the time of their current appointment.
In terms of their work life, 30.4% of the individuals reported that their disease did not affect their work. The biggest concern for 59.6% of the patients was the potential of their condition worsening and impacting their lives. Additionally, 17% of the patients were hesitant to disclose their diagnosis to friends and family. The most common issue affecting their social life was psoriasis, reported by 19.7% of the patients.
38.4% of the participants expressed confidence in future improvement in their condition, 30.8% were not optimistic, and 30.8% were uncertain.
Conclusion: These findings emphasize the need for standardized protocols, more awareness of the disease among patients, and a systematic pathway to prevent diagnosis delay and improve patient care in initial consultations for PsA. Significant frequent changes in healthcare providers post-diagnosis were highlighted, indicating the need for improvement.
To cite this abstract in AMA style:
Azman F, Tanin K, Sacin E, Azman E, Rizaoglu M, Uc C, Acar B, Ugurlu S. The Journey of a Patient with Psoriatic Arthritis: The Path from Diagnosis to Treatment [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/the-journey-of-a-patient-with-psoriatic-arthritis-the-path-from-diagnosis-to-treatment/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-journey-of-a-patient-with-psoriatic-arthritis-the-path-from-diagnosis-to-treatment/