Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Type 2 SLE symptoms of fatigue, widespread pain, sleep and cognitive dysfunction occur commonly in SLE although their etiology is unknown. Since trauma has been associated with chronic pain, depression, and anxiety in SLE, the aim of this study was to assess the relationship between trauma and features of Type 2 SLE.
Methods: Adult SLE patients (2012 SLICC or 2019 ACR/EULAR criteria) enrolled in a prospective academic lupus registry completed the polysymptomatic distress scale and level of anxiety at each clinic visit. The rheumatologist scored the Type 1 and Type 2 PGA (physician’s global assessment), a 3-point visual analog scale assessing Type 1 and 2 SLE activity respectively. Patient responses to the Brief Trauma Questionnaire with additional questions regarding emotional abuse, severe illness in a child or infant, and pregnancy loss, abortion, and complications were captured during a routine visit. Type 2 medications included antidepressants, gabapentin, pregabalin, muscle relaxers topiramate, sleep medications, stimulants, and DHEA. Patients were grouped into 3 groups: no trauma, abusive and non-abusive trauma. Abusive trauma included physical, sexual, and emotional trauma as an adult or child. Differences across groups were analyzed by Fisher’s exact test or ANOVA.
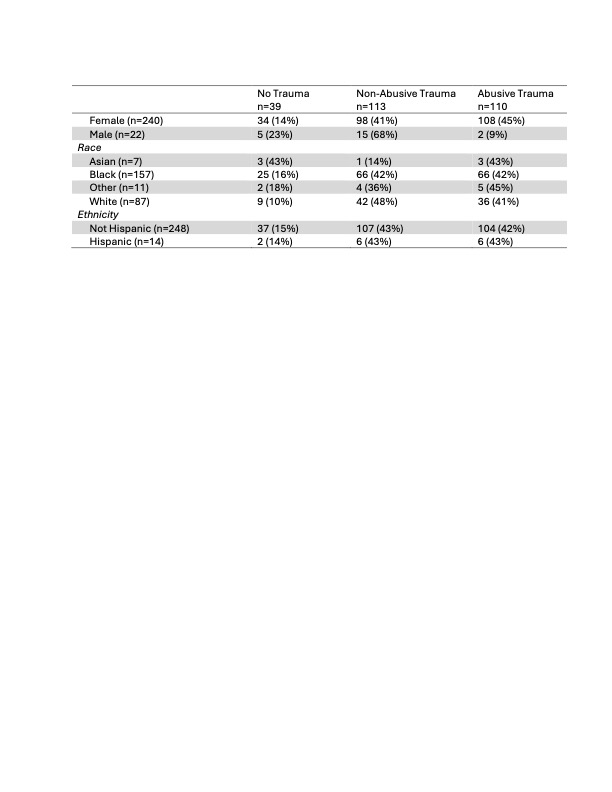
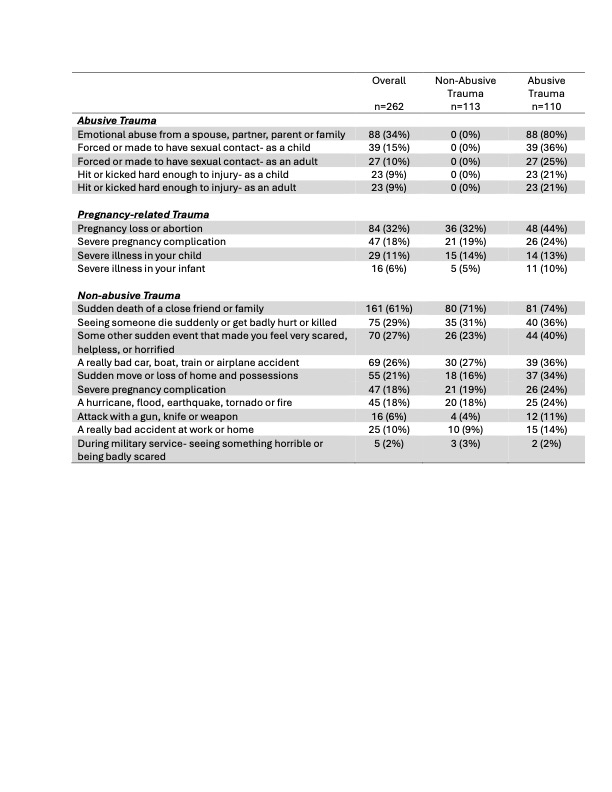
Results: In this study of 262 SLE patients (92% female, mean age 44 years, mean disease duration 15 years), 85% of patients reported trauma with a mean number of 3 types occurring a median of 6 times, excluding 14% of patients with trauma too frequent to count. Women were five times more likely be victims of abusive trauma than men (Table 1). The sudden loss of family or friend was the most commonly reported trauma (61%), followed by emotional abuse (34%) and pregnancy loss or abortion (32%) (Table 2). Patients with a history of abusive trauma were more likely to suffer all other types of trauma except for military events.
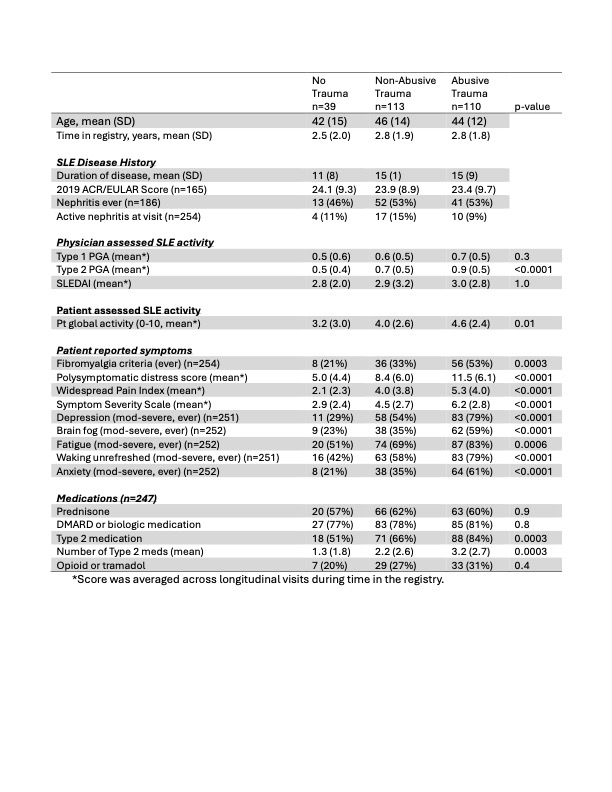
The burden of Type 2 SLE was greatest in those with abusive trauma (Table 3). Patients with abusive trauma had higher mean Type 2 PGA scores and were significantly more likely to have fibromyalgia and report fatigue, depression, brain fog, unrefreshed sleep and anxiety compared to those without trauma. More patients with abusive trauma were prescribed Type 2 SLE medications and in larger numbers than the other groups. There was no difference in the frequency of Type 1 SLE, however, as measured by total ACR/EULAR scores, nephritis, mean SLEDAI or Type 1 PGA across groups. Likewise, the use of prednisone, DMARDs and biologics was similar across groups.
Conclusion: These findings suggest that a history of trauma is highly prevalent in SLE and is associated with mood disorders and symptoms of Type 2 SLE, with those with abusive trauma experiencing the greatest degree of symptoms over time. Trauma was not associated with cumulative Type 1 SLE activity, however. A patient’s trauma history may contribute to symptoms considered as Type 2 SLE and poor health related quality of life. Ascertaining a trauma history during patient evaluation may help guide a patient-centric approach to care.
To cite this abstract in AMA style:
Rogers J, Clowse M, Pisetsky D, Doss J, Maheswaranathan M, Criscione-Schreiber L, Sadun R, Sun K, Eudy A. The Influence of Trauma on Features of Type 2 SLE [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/the-influence-of-trauma-on-features-of-type-2-sle/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-influence-of-trauma-on-features-of-type-2-sle/