Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: The 2017 guidelines by the American College of Cardiology/American Heart Association (ACC/AHA) define hypertension at a threshold of ≥130/80mmHg for the systolic and diastolic blood pressure (SBP, DBP) respectively instead of ≥140/90mmHg. Studies in patients with systemic autoimmune diseases, where BP is fluctuating over time due to various reasons, were not considered. The aim of the present study was to assess the impact of the new definitions on the prevalence and incidence of atherosclerotic cardiovascular events (CVEs) in systemic lupus erythematosus (SLE).
Methods: Patients from the Lupus Clinic with at least two years of follow-up and no previous atherosclerotic CVEs were included. Since the blood pressure (BP) in lupus patients varies particularly in the early phases, we calculated the adjusted mean BP over the first two years and divided the patients into three groups (≥140/90mmHg, 130-139/80-89mmHg and < 130/80mmHg). Patients were followed until the first occurrence of a CVE (new onset of: angina, myocardial infarction, congestive heart failure, coronary angioplasty or by-pass graft, transient ischemic attack, stroke and cardiovascular death) or the last visit. Prevalence and incidence rates of CVEs were calculated separately for each group. SAS 9.4 was used for statistics (time-to-event analysis); p< 0.05 was considered significant.
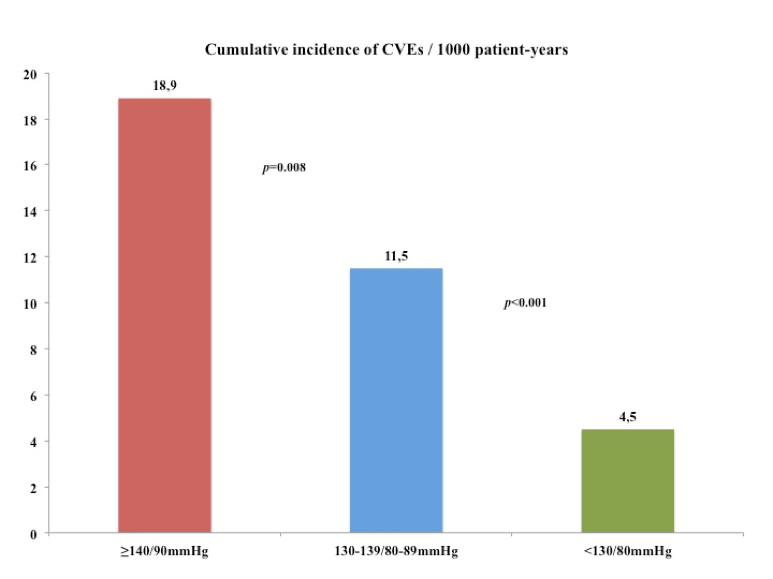
Results: 1532 patients satisfied the inclusion criteria (88.1% females, mean age at baseline 36.2±14.3 years, mean disease duration 6.1±6.3 years). The prevalence of hypertension by the previous definition was 10.1% (155/1532) and with the current definition 30.7% (471/1532); the rest 1061 (69.3%) were normotensives. After a mean follow-up of 10.8 years, there were 124 CVEs (104 non-fatal and 20 fatal) among all patients. The total prevalence of CVEs in the three groups was 32/155 (20.6%) in the ≥140/90mmHg, 41/316 (13%) in the 130-139/80-89mmHg and 51/1061 (4.8%) in the normotensive group, respectively. The cumulative incidence per 1000 patient-years is shown in Figure 1. Similar trends (gradually increasing incidence rates from the normotensives to the 130-139/80-89mmHg and the ≥140/90mmHg groups) were found individually for the coronary artery disease (CAD) events, cerebrovascular events and cardiovascular deaths.
Conclusion: SLE patients with an adjusted mean BP of 130-139/80-89mmHg over two years developed approximately 2.5fold more CVEs compared to normotensive patients. The new definition of hypertension highlights a group of patients with a high incidence of CVEs who should be targeted for more intensive therapy in order to improve cardiovascular outcomes.
To cite this abstract in AMA style:
Tselios K, Gladman D, Su J, Urowitz M. The Impact of the New American College of Cardiology/American Heart Association Definition of Hypertension on Cardiovascular Events in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-impact-of-the-new-american-college-of-cardiology-american-heart-association-definition-of-hypertension-on-cardiovascular-events-in-systemic-lupus-erythematosus/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-the-new-american-college-of-cardiology-american-heart-association-definition-of-hypertension-on-cardiovascular-events-in-systemic-lupus-erythematosus/