Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: PAPS is an autoimmune disease marked by thrombosis, obstetric poor outcomes and antiphospholipid antibodies. Despite treatment, APS is associated with high morbidity and mortality, mainly from thrombotic events and cardiovascular risk factors (CVRF). This study evaluates the corelation between sedentary time, physical activity and clinical parameters in PAPS.
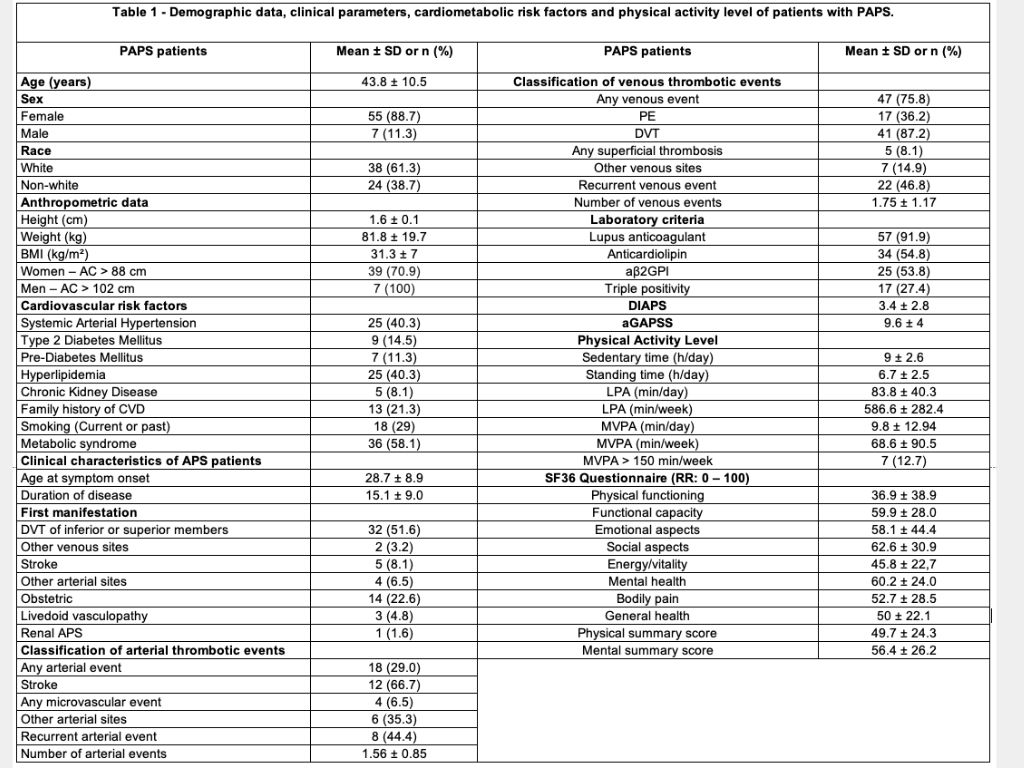
Methods: This cross-sectional study included 62 patients with thrombotic PAPS classified by Sydney criteria (1), without severe physical limitations. Sedentary time and physical activity were measured using activPALmicro™ accelerometers over 7 days and analyzed with ActivPAL3™ software. Variables included time spent in sedentary behavior, sitting/lying, light physical activity (LPA), and moderate to vigorous physical activity (MVPA). Thrombotic risk was evaluated using the Adjusted Global AntiPhospholipid Syndrome Score (aGAPSS), damage by the Damage Index in APS (DIAPS) and quality of life with the SF-36 questionnaire. Descriptive statistics were calculated as mean ± standard deviation and percentages. Normality was tested with the Shapiro-Wilk test. Mann-Whitney and Spearman correlation tests were used. Multiple linear regression models were proposed. Analyzes were performed with 5% significance level using Jamovi and R.
Results: Table 1 summarizes data in PAPS patients, predominantly female (89%), with age of 43.8±10.5years and BMI of 31.3±7 kg/m². CVRF included hypertension (40%) dyslipidemia (40%) and BMI over 30kg/m² (53,2%). Most patients were positive for lupus anticoagulant (92%), with 27% having triple positivity. PAPS DIAPS was 3.4±2.8 and aGAPSS was 9.6±4. Patients presented 9±2.6h of daily sedentary time, with only 12.7% meeting the recommended 150min of weekly MVPA. No significant correlations were found between sedentary time, physical activity levels and aGAPSS scores. Patients with higher thrombosis recurrence presented lower standing time (p=0.006) and a tendency towards longer sedentary time (p=0.059).
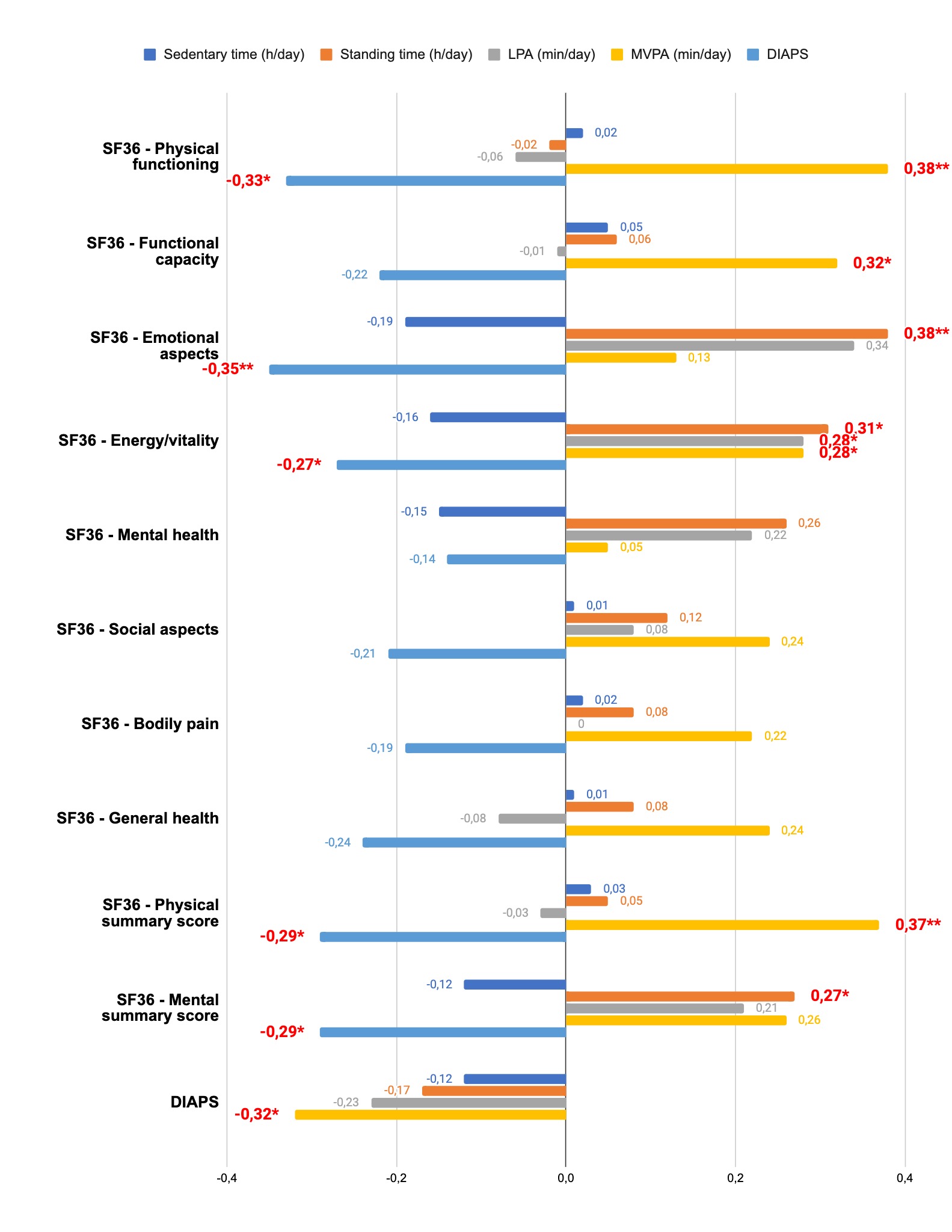
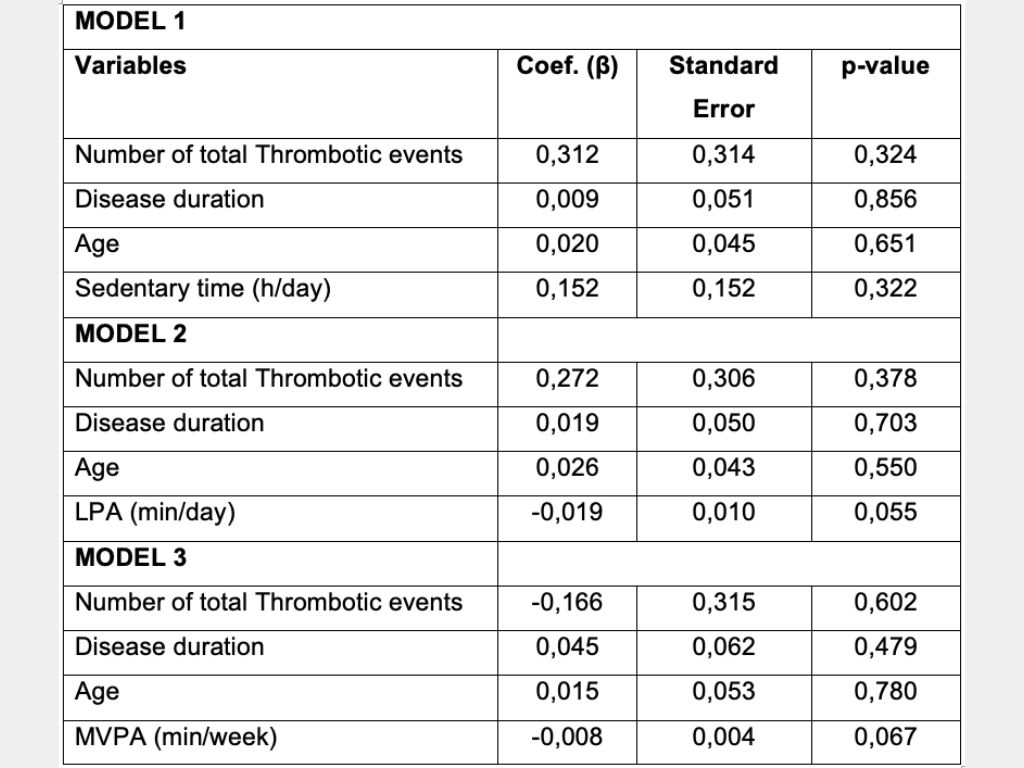
DIAPS was negatively correlated with higher MPVA (p< 0.05; rho= -0.32) and with SF-36 domains: physical (rho= -0.33), emotional (rho= -0.35), energy/vitality (rho= -0.27), physical (rho= -0.29), and mental (rho= -0.29) scores (Fig 1). Positive correlations (p< 0.05) were found between MVPA and SF-36 domains: physical aspect (rho= 0.38), functional capacity (rho=0.32), energy/vitality (rho=0.28), and physical aspect (rho=0.37) (Fig 1). In the multiple linear regression model (table 2) between independent variables and DIAPS, physical activity showed a trend towards damage reduction: LPA might affect DIAPS (β= -0.019, p=0.055) and MVPA negatively (β= -0.008, p=0.067).
Conclusion: This study suggests a correlation between physical activity and better health outcomes in PAPS. Higher levels of MVPA were inversely associated with DIAPS, and increased physical activity improved the perception of quality of life. This study suggests that PAPS should be oriented to remain active.
To cite this abstract in AMA style:
Silva C, Andrade D. The Impact of Sedentary Behavior and Physical Activity Level on Clinical Parameters and Quality of Life in Patients with Primary Antiphospholipid Syndrome (PAPS) [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/the-impact-of-sedentary-behavior-and-physical-activity-level-on-clinical-parameters-and-quality-of-life-in-patients-with-primary-antiphospholipid-syndrome-paps/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-sedentary-behavior-and-physical-activity-level-on-clinical-parameters-and-quality-of-life-in-patients-with-primary-antiphospholipid-syndrome-paps/