Session Information
Session Type: Abstract Session
Session Time: 4:00PM-5:30PM
Background/Purpose: To minimize risk of poor pregnancy outcomes, the ACR Reproductive Health Guideline recommends women conceive when SLE is well controlled and treated with pregnancy-compatible medications. In addition to SLE disease activity and medications, social determinants of health can impact pregnancy outcomes. We studied the association between pregnancy timing, social determinants of health, and pregnancy outcomes.
Methods: All study participants met SLICC criteria for SLE, were pregnant, and enrolled in a prospective registry. At baseline, patients reported social determinants of health and SLE activity; medications, laboratory results, and physician-assessments of SLE activity were also recorded. Pregnancy timing was defined in 3 ways based on whether the woman was medically optimized, the woman intended to become pregnant, or both. “Medically optimized” pregnancies met the following criteria: no teratogen use, continued pregnancy-compatible SLE medications, and urine protein:creatinine ratio (UPC) < 1g in the 6 months prior to or during the first trimester. “Intended” pregnancies were defined using the London Measure of Unplanned Pregnancy (LMUP), a validated, 6-question self-reported survey assessing the extent that the woman intended to become pregnant. Well-timed pregnancies were both medically optimized and intended; ill-timed were either not medically optimized and/or intended. Statistical analyses compared differences in outcomes by our three definitions of pregnancy timing.
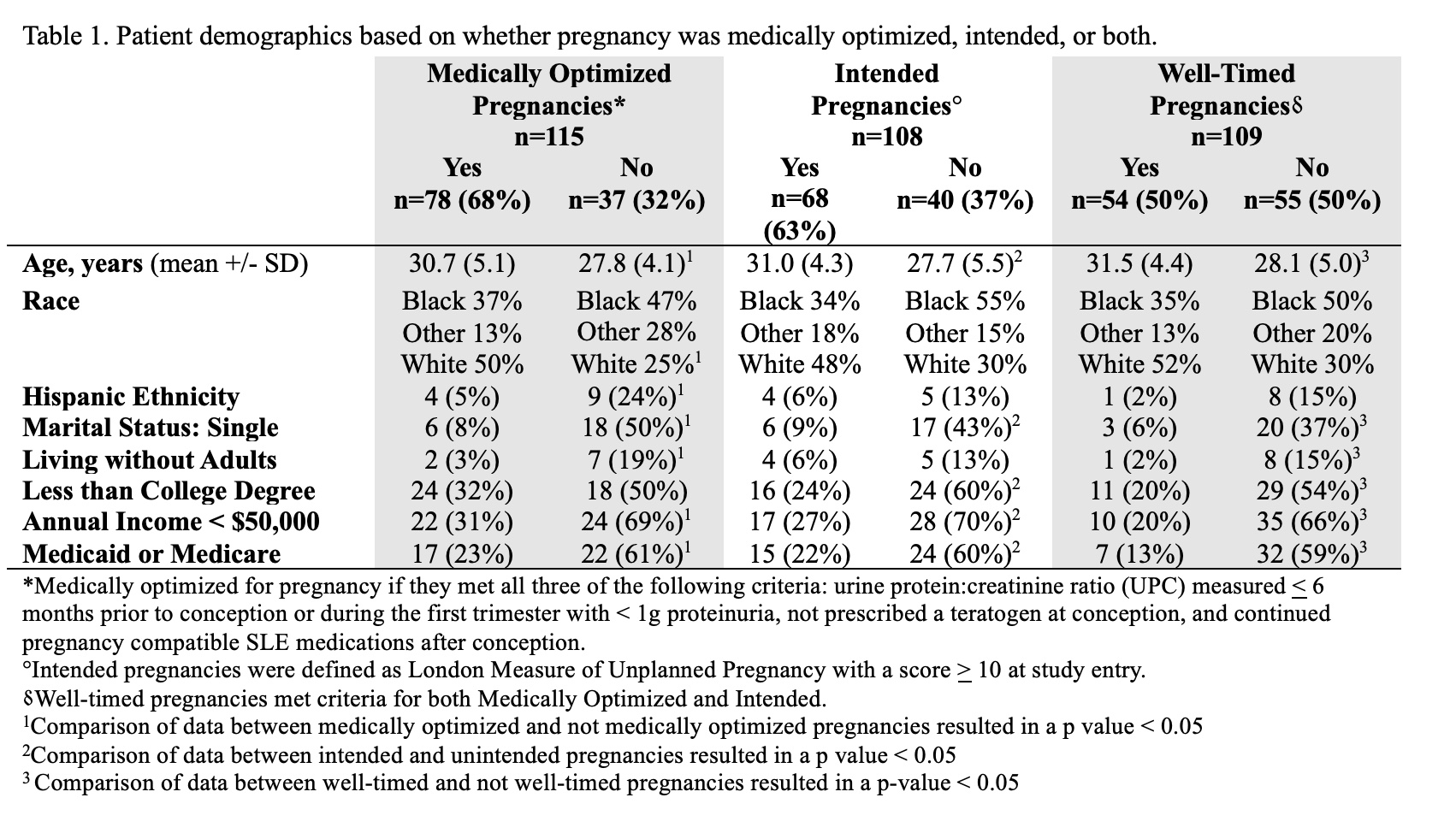
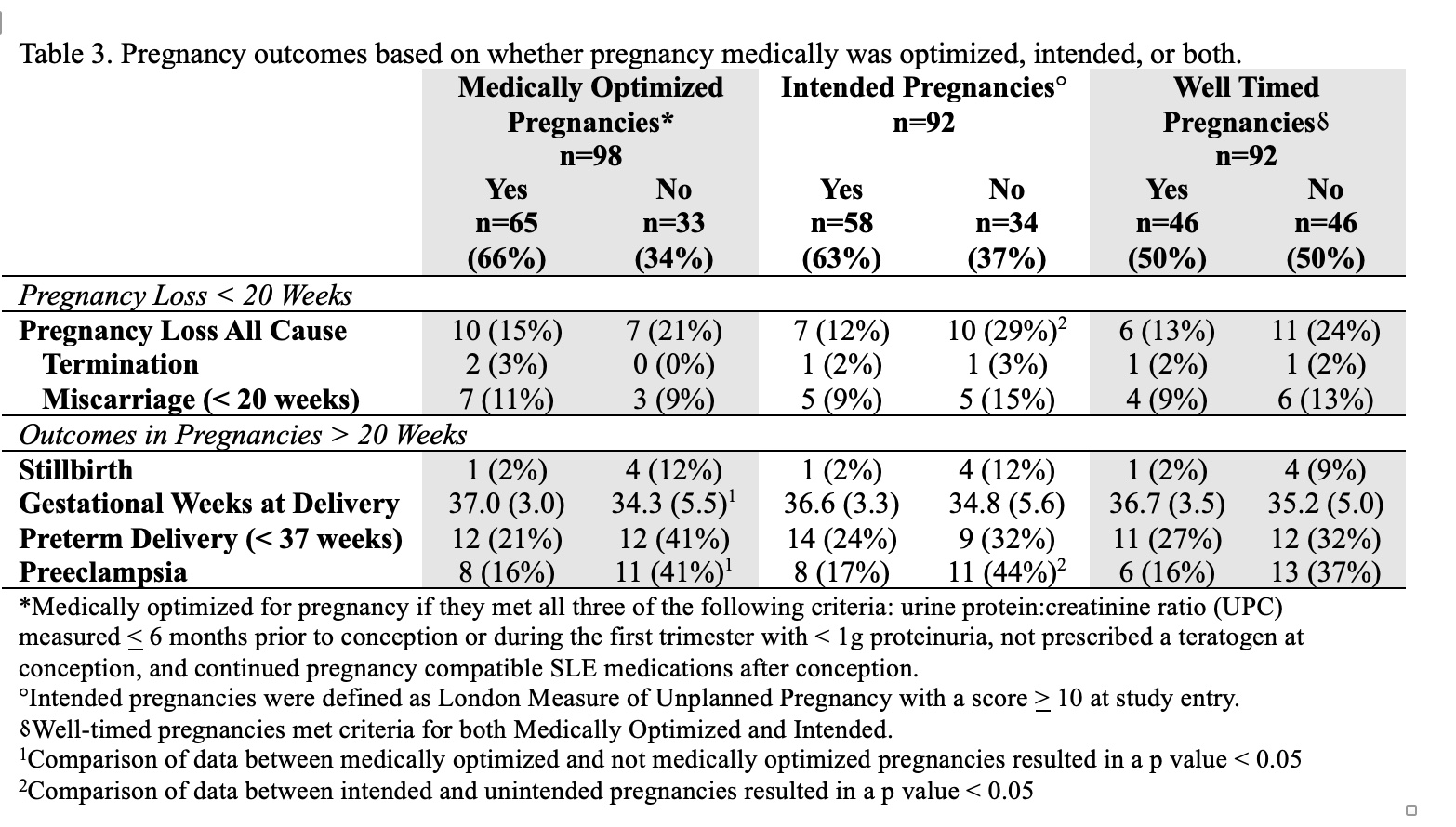
Results: A total of 115 women were enrolled, with half of pregnancies both intended and medically optimized, 20% neither intended nor medically optimized, 17% not intended but medically optimized, and 13% intended but not medically optimized. Ill-timed pregnancies were more likely to be conceived by women who were single, identify as Black or Hispanic, receive Medicaid or Medicare, have a lower income and level of education (Table 1). Additionally, women with ill-timed pregnancy had higher physician-reported SLE disease activity, were less likely to be taking pregnancy-compatible medications at their initial pregnancy visit and more likely to be taking mycophenolate at conception (Table 2). Ill-timed pregnancies were more likely to end with preeclampsia and early delivery (Table 3). In pregnancies that were not medically optimized, when adjusted for marital status, low income, Medicaid or Medicare, the risk of preterm birth and preeclampsia was three times higher than in medially optimized pregnancies (AOR: 3.33; 95% CI: 1.06, 10 for preterm birth and AOR: 3.0; 95% CI: 0.95, 10 for preeclampsia). These pregnancies were, on average, more than two weeks shorter (adjusted β: -2.38; 95% CI: -4.42, -0.34).
Conclusion: In this cohort of pregnant patients with SLE, women with ill-timed pregnancies, whether because she didn’t intend to be pregnant or was not medically optimized for pregnancy, had multiple factors contributing to their higher risk for poor pregnancy outcomes, including social disadvantage, increased lupus activity, and inappropriate medication use. In order to improve outcomes in SLE, we need to target specific interventions to this particularly vulnerable population.
To cite this abstract in AMA style:
Sims C, Eudy A, Harding C, Edens C, Birru Talabi M, Ramsey-Goldman R, Neil L, Clowse M. The Impact of Pregnancy Timing on Outcomes in SLE [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/the-impact-of-pregnancy-timing-on-outcomes-in-sle/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-pregnancy-timing-on-outcomes-in-sle/