Session Information
Date: Monday, November 13, 2023
Title: (1345–1364) Reproductive Issues in Rheumatic Disorders Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Mental health conditions are the leading cause of maternal mortality across most of the United States. Among individuals with SLE, pregnancy intention has been noted as a risk factor for adverse pregnancy outcomes and infant complications. However, the impact of pregnancy intention on maternal mental health and quality of life in this population is poorly understood.
Methods: We conducted a prospective cohort study using data from a university-based pregnancy registry that enrolls pregnant women with rheumatic disease. Patient reported outcomes including the London Measure of Unplanned Pregnancy (LMUP) and Edinburgh Postnatal Depression Scale (EPDS) were collected at first rheumatology visit of pregnancy. The EPDS is validated in pregnancy. Data for patient measures and physician assessed SLE activity were obtained at each subsequent visit. Pregnancy intention was stratified into two categories: (1) Planned versus unplanned based on LMUP≥10 and (2) Medically optimized versus not optimized. Medically optimized for pregnancy was defined as < 1g of proteinuria, no rheumatic teratogens at conception, and continuing pregnancy compatible SLE medications after conception. We conducted primary and secondary analyses using Fisher’s exact test to estimate the association of pregnancy intention with maternal depression, maternal mental health/quality of life, and maternal SLE activity. Multivariable logistic regression models were used to estimate the association of pregnancy intention with each outcome of interest.
Results:
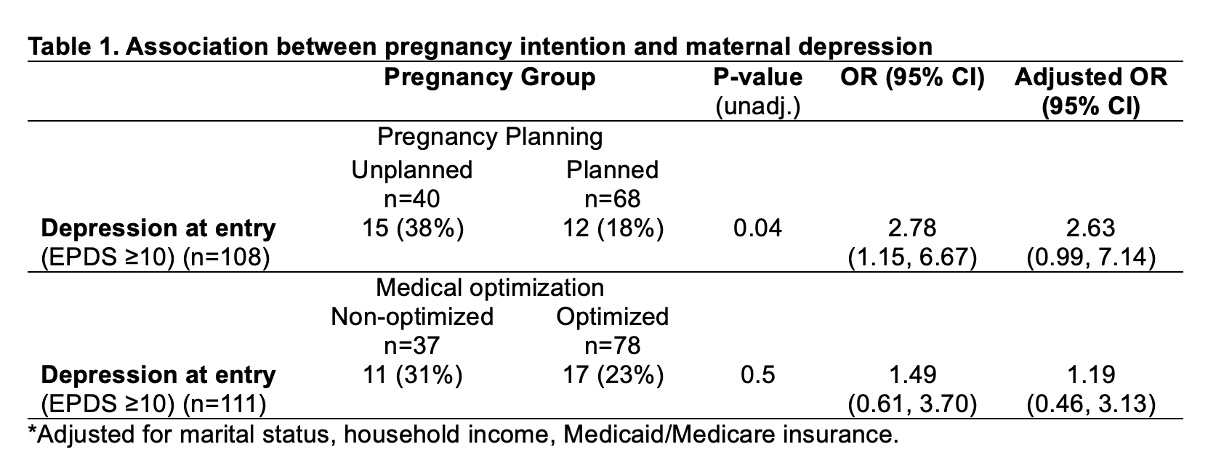
Depression: Individuals with unplanned pregnancy were 2-3 times as likely to have maternal depression as those with planned pregnancy. On the other hand, individuals who were not medically optimized for pregnancy did not have a significant increase in depression (Table 1).
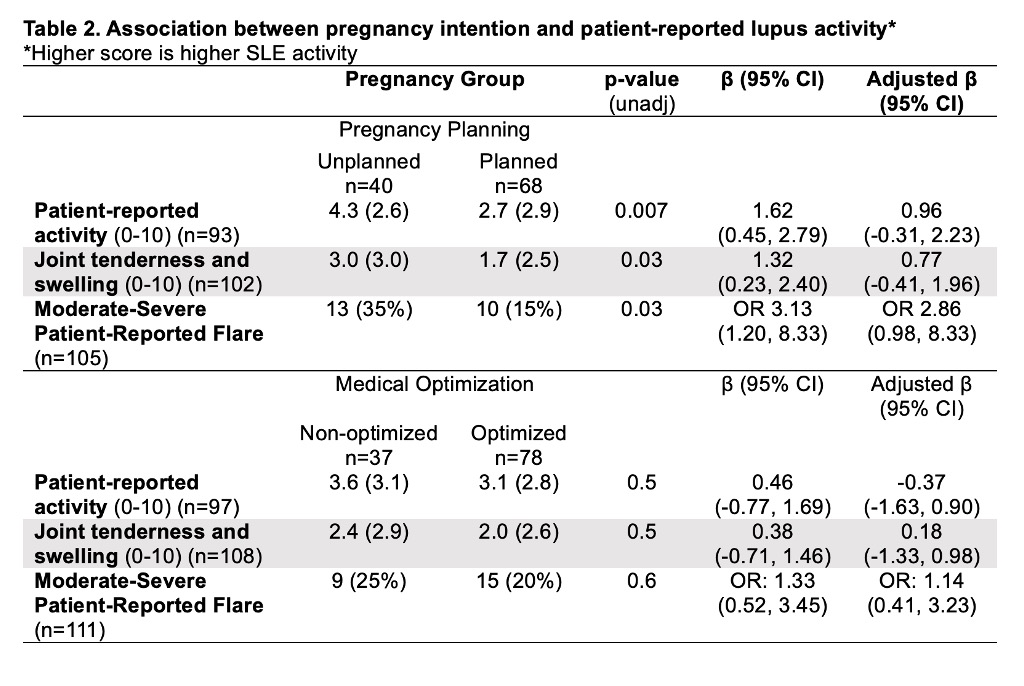
Patient-reported SLE activity: Higher patient-reported lupus activity was seen in unplanned pregnancy than in planned pregnancy, with three-times as many reporting a moderate or severe flare. However, patient-reported lupus activity was not associated with whether or not pregnancy was medically optimized (Table 2).
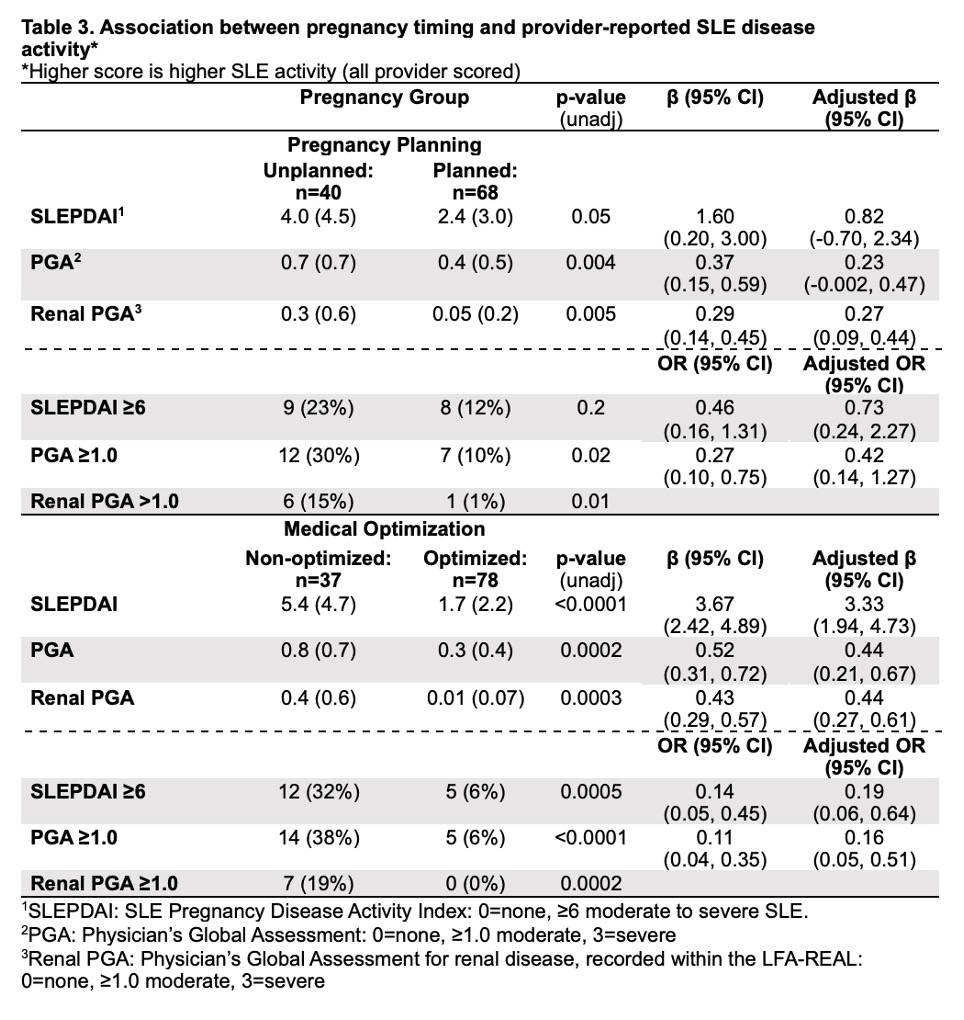
Physician-reported SLE activity: When adjusted for marital status, household income, and Medicaid/Medicare insurance, unplanned pregnancies did not have higher SLE activity, despite higher patient-reported symptoms (Table 3).On the other hand, pregnancies that were not medically optimized had significantly higher rates of active SLE, SLEPDAI, and active nephritis, even though the women did not report higher SLE activity.
Conclusion: Early in pregnancy, maternal depression and patient-reported SLE symptoms were associated with unplanned pregnancy, but not whether SLE activity or medications were optimized in pregnancy. On the other hand, physician-reported SLE activity, which is an important predictor of pregnancy outcomes, was not increased in unplanned pregnancies, but was higher in pregnancies not medically optimized. These results suggest that addressing unplanned pregnancy may improve maternal mental health, and increasing medical optimization prior to conception may have more impact on pregnancy outcomes.
To cite this abstract in AMA style:
Harding C, Eudy A, Sims C, Edens C, Birru Talabi M, Ramsey-Goldman R, Neil L, Clowse M. The Impact of Pregnancy Intention on Depression and Quality of Life in Women with Lupus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/the-impact-of-pregnancy-intention-on-depression-and-quality-of-life-in-women-with-lupus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-pregnancy-intention-on-depression-and-quality-of-life-in-women-with-lupus/