Session Information
Date: Saturday, November 6, 2021
Title: Patient Outcomes, Preferences, & Attitudes Poster I: Impact (0225–0240)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Rheumatic diseases, such as SLE, are associated with serious maternal, pregnancy, and infant complications. The role that preeclampsia plays in these outcomes in women with SLE and other rheumatic disease remains unclear. We compared pregnancy and infant outcomes among women with SLE and other rheumatic diseases with and without preeclampsia in a single academic center.
Methods: Deliveries in women with rheumatic disease were identified from both a prospective cohort of women with rheumatic disease who received care within a university rheumatology clinic and a chart-reviewed list of deliveries to women with an ICD-9/10 code for SLE. Mothers with rheumatic disease were matched with their infants through the electronic medical record (EMR) to allow data extraction. Preeclampsia was determined by the obstetric team at the time of delivery and collected through chart review. Pregnancy and infant outcomes were compared between those with and without preeclampsia.
Results: 263 singleton deliveries were included in the study of whom 14% had preeclampsia. Preeclampsia was significantly more common among women with SLE than with other rheumatic diseases (SLE 27% vs other rheumatic diagnoses 8%, p< 0.001); this pattern persisted among both Black and White women and women with private health insurance. Among women with SLE, however, the rate of preeclampsia was similar between Black and White women and those with and without private insurance. Having preeclampsia increased the mother’s hospital stay for delivery by an average of 2 days for women with SLE and 1 day for women with other rheumatic diseases.
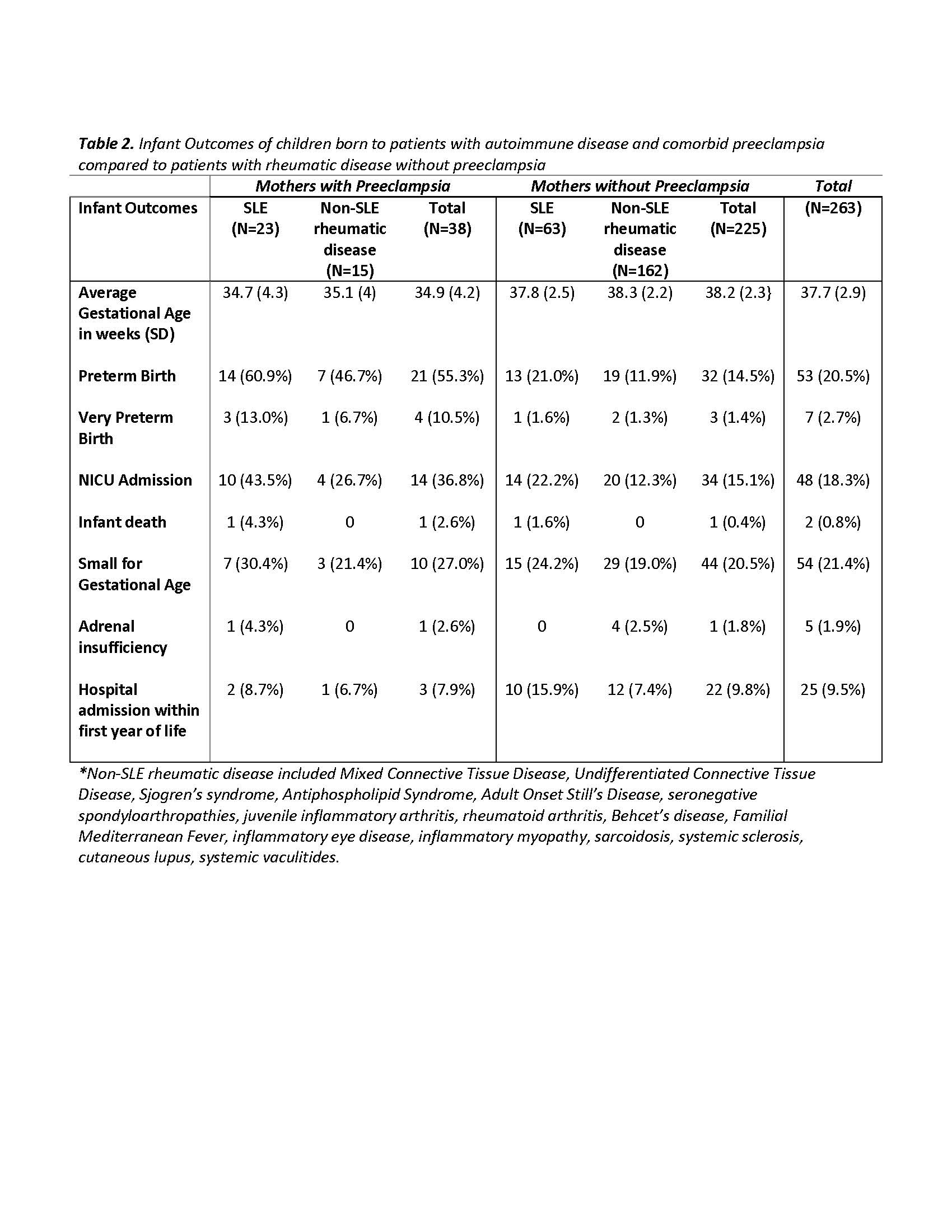
Infants born to preeclamptic mothers were delivered an average of 3.3-weeks earlier than those without preeclampsia; they were 4-times more likely to be born preterm (55.3% vs 14.5%, p< 0.001), a difference that persisted in mothers with SLE and other rheumatic diagnoses. More than twice as many infants born to preeclamptic mothers were admitted to the neonatal intensive care unit (NICU; 36.8% vs 15.1%, p< 0.0001). While infants born to women with SLE without preeclampsia had modestly higher rates of preterm birth and NICU admission compared to women with other rheumatic diseases, preeclampsia drove these rates significantly higher in all women.
Conclusion: Preeclampsia has important health consequences on mothers with rheumatic disease, including increasing hospitalization at delivery by 1-2 days, and on the infant, increasing the frequency of preterm delivery and NICU admission. Preeclampsia was particularly common among women with SLE in this cohort. These data suggest that preventing preeclampsia could have a dramatic impact on the short- and long-term health of women with rheumatic disease and their children.
To cite this abstract in AMA style:
Milne M, Clowse M, Eudy A, Zhao C, Goldstein B. The Impact of Preeclampsia on Pregnancies and Infants of Women with Rheumatic Disease [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/the-impact-of-preeclampsia-on-pregnancies-and-infants-of-women-with-rheumatic-disease/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-preeclampsia-on-pregnancies-and-infants-of-women-with-rheumatic-disease/