Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Factors such as menopause, hormonal replacement therapy (HRT), oral contraceptives (OC), pregnancy, and breast-feeding have been associated with the risk of developing Rheumatoid Arthritis (RA) in women. However, the effect of these factors on RA disease progression has had little investigation.
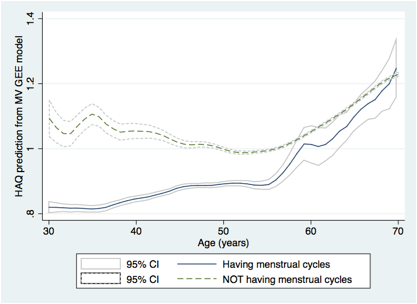
Methods: Using a large US observational cohort, the National Data Bank for Rheumatic Diseases, we investigated the impact of menopause on RA functional outcomes as measured by the Heath Assessment Questionnaire (HAQ) and HAQ annual progression rates. We excluded all women who went through menopause before RA onset. Menopausal status (1=menstruating, 0=reached menopause) was further analyzed by comparing 3 groups of women based on their menopausal status while under observation in the study: premenopausal, post-menopausal, & transitioned through menopause. Possible confounders controlled for included age, educational level, household income, use of anti-TNF agents, HRT, and OC. We used univariate and multivariate (MV) generalized estimating equations (GEE) methods with the sandwich estimator. To account for a possible non-linear relationship between age and HAQ, we used a cubic spline with 3 knots at age 40, 56, 72, and an interaction term. Best models were selected using the QIC_u criterion.
Results: A total of 7,632 women were eligible between 1998 and 2012 with an average of 2.9 years in the study. Of these, 2,102 were premenopausal (28%), 618 underwent menopause (8%), and 4,912 were entirely post-menopausal (64%). Within each respective group, the mean (SD) ages were 40 (8.2), 51 (SD 6.1), and 61 (9.9) years. Our results showed that women who were still having menstrual cycles tended to have a better HAQ score by -0.33 (-0.52, -0.14) than women who stopped having menstrual cycles; these results were robust even after full adjustment for other significant factors, -0.32 (-0.51, -0.14) (see Figure). The use of OC ever in reproductive life seemed also protective for disability as well as having had a pregnancy. On the other hand, HRT did not seem to be associated with disability. HRT and pregnancy did not qualify by our criterion for the final multivariate model. Using the menopause status with the 3 groups in the full model, in comparison with pre-menopausal women, HAQ of post-menopausal women were increased by 0.51 (0.16, 0.85), and not differ for who underwent menopause, 0.038 (-0.26, 0.33). The HAQ rate of progression was -0.001 per year (-0.248, 0.117) when comparing women who reached menopause with those who didn’t.
Conclusion: In this large observation study, our results suggest that higher levels of estrogen may be associated with reduced functional limitations. However, HAQ progression continued similarly post-menopause as it did pre-menopause.
Disclosure:
S. Pedro,
National Data Bank for Rheumatic diseases,
3;
E. Chakravarty,
None;
M. E. B. Clowse,
UCB,
5;
R. Schumacher,
National Data Bank for Rheumatic diseases,
3;
K. Michaud,
National Data Bank Bank & University of Nebraska Medical Center,
3.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-menopause-in-rheumatoid-arthritis-activity/