Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
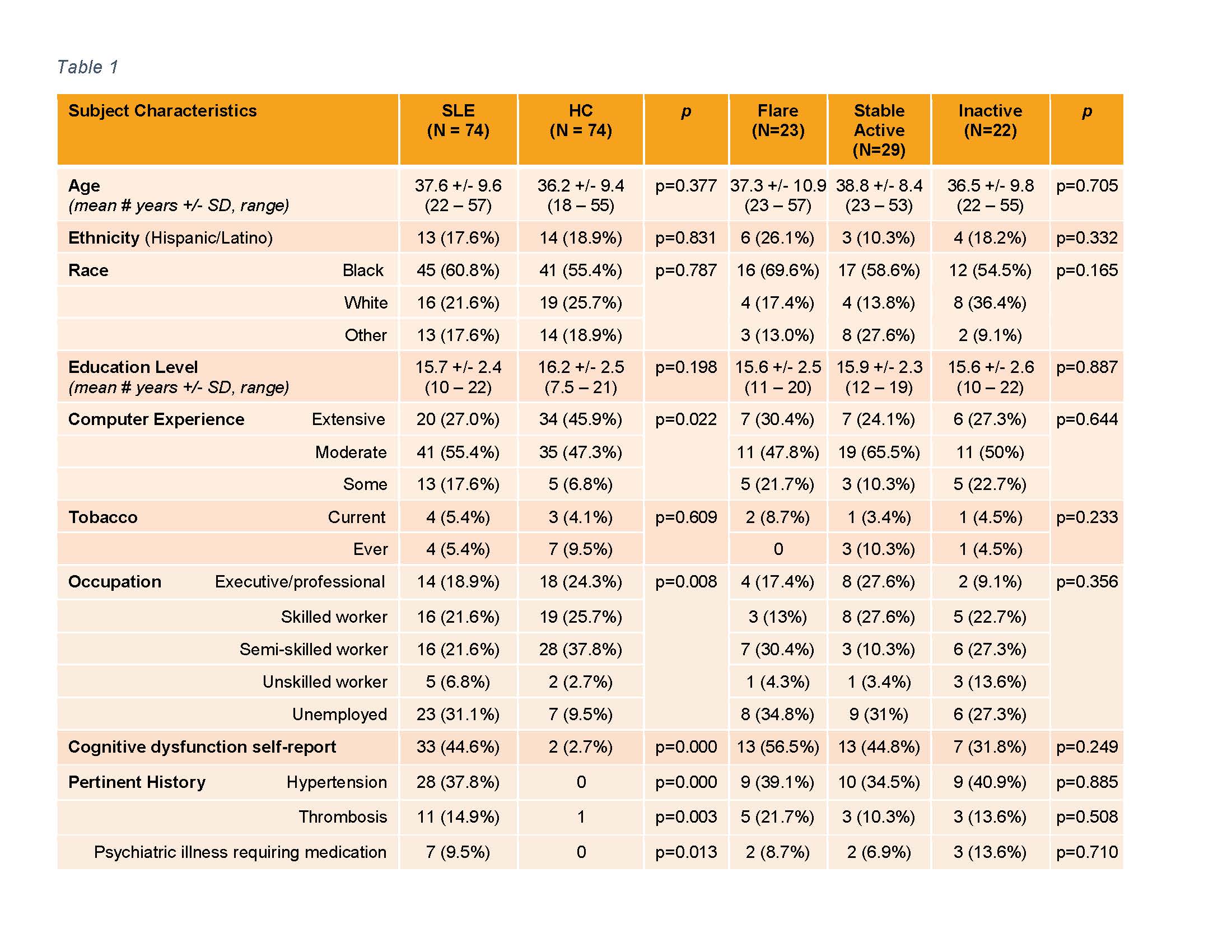
Background/Purpose: Attribution of cognitive dysfunction (CD) to SLE is compromised by potential confounders. Studies reveal conflicting results on the relationship between CD and disease activity, likely due to testing differences, subject demographics, comorbidities (NPSLE in particular), and small sample sizes. We assessed cognition in a large cohort of SLE subjects compared to healthy controls (HC) to determine the impact of disease activity.
Methods: Seventy-four adult SLE subjects that met ACR criteria, had no history of NPSLE or other CNS deficits, and 74 age, gender and racially matched HC underwent cognitive testing and assessments for depression, pain, fatigue, sleepiness, anxiety and anger. SLE subjects were assessed for disease activity and medication use. Exclusion criteria included alcohol or illicit drug dependence/abuse, infection, and current narcotic/psychiatric medication use. SLE disease activity status was categorized as “Flare” (met SELENA SLEDAI Flare Index criteria), “Stable active” [clinical SLEDAI (all descriptors other than serology) > 0 or PGA > 0.5 or prednisone > 10 mg and lack of flare], and “Inactive” (clinical SLEDAI = 0 and PGA ≤ 0.5 and prednisone ≤ 10 mg and lack of flare). Differences in group characteristics and test performance were assessed between SLE and HC (t-test and/or Mann Whitney), and among the SLE disease activity groups (ANOVA with post-hoc Tukey’s). The impact of variables on individual test performance was determined by multivariable modeling for SLE versus HC and SLE only grouped by disease activity; variables on univariate screen (p< 0.1) were included.
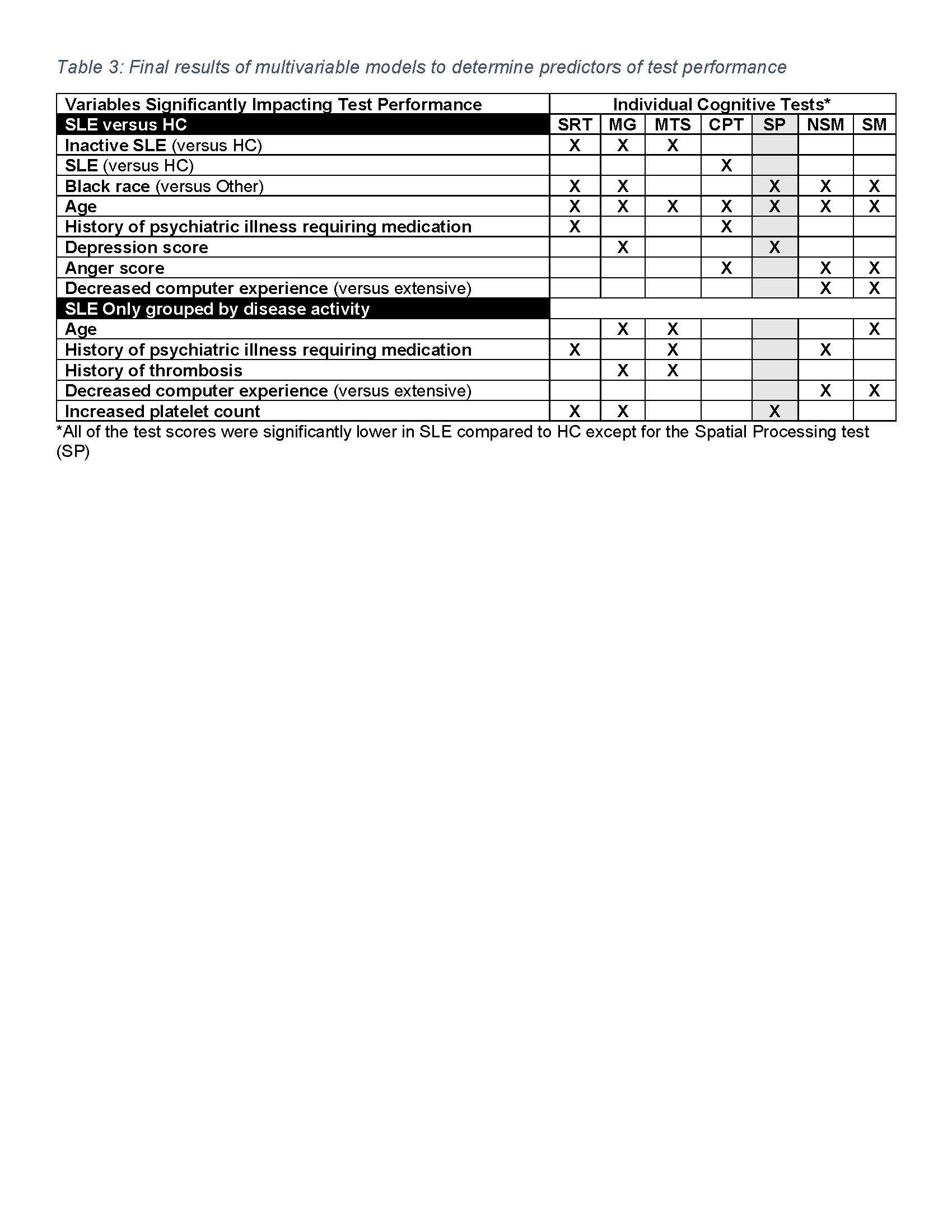
Results: There were no demographic differences among SLE and HC groups (Table 1). Compared to HC, SLE scored worse on most tests and this poor performance was driven by increased reaction time rather than poor accuracy for most tests (Table 2). Among SLE subjects, disease activity did not impact test performance; unexpectedly, inactive SLE performed the worst compared to HC (Table 2). Multivariable models demonstrate significant impacts of 1) SLE, age (as expected), Black race, depression, anger, computer experience and history of psychiatric illness in SLE versus HC and 2) age, increased platelets, history of psychiatric illness, computer experience and history of thrombosis in SLE only (Table 3).
Conclusion: Multivariable analyses suggest that poor cognitive performance is related to having SLE after controlling for other factors. Surprisingly, disease activity did not associate with performance, and unpredicted variables such as Black race, increased platelets, history of thrombosis and psychiatric illness did. Black race may be a surrogate for socioeconomic status. The potential of platelets as contributors to other neurodegenerative disease(1) supports further investigation in SLE. The paucity of associations between SLE cognitive performance and disease measures demonstrated in this study highlights the importance of continued study of biologic neurotoxic mechanisms for CD.
- Pluta R, Ulamek-Koziol M, Januszewski S, Czuczwar SJ. Platelets, lymphocytes and erythrocytes from Alzheimer’s disease patients: the quest for blood cell-based biomarkers. Folia Neuropathol. 2018;56(1):14-20.
To cite this abstract in AMA style:
Anderson E, Ploran E, Hong J, Diamond B, Volpe B, Aranow C, Mackay M. The Impact of Disease Activity and Related Factors on Cognitive Dysfunction in SLE [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-impact-of-disease-activity-and-related-factors-on-cognitive-dysfunction-in-sle/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-disease-activity-and-related-factors-on-cognitive-dysfunction-in-sle/