Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Value based health care has gained worldwide attention due to the refocusing vision of creating value around and for patients. The latter is obtained by measuring healthcare outcomes/quality relative to the cost. Besides measuring these parameters, another crucial element in the evaluation of value-based reimbursement decisions depends on adequate registration. Therefore, in this study we aimed to objectify the degree of misregistration by comparing the received diagnosis of rheumatoid arthritis from a rheumatologist-driven, scientific (ACR/EULAR-2010 criteria for RA), and financial (ICD-10) perspective.
Methods: All patients who received the diagnosis Rheumatoid Arthritis (RA) between 2000-2016 within our hospital, were identified according to the Diagnosis Treatment Code (DTC) RA, which is a financial instrument that corresponds to the ICD-10 system (corresponding codes for RA: ICD-10 M05.79/M05.89/M06.09/M06.89). Clinical and demographic data were extracted from digital patient records in which 10% of the data were randomly cross-checked. The collected variables at time of RA diagnosis included number and type of swollen/painful joints, inflammatory markers, rheumatoid factor (RF), ACPA, disease duration and patients primary/secondary/tertiary diagnosis according to the rheumatologist. Additionally, patients were classified according to the ACR/EULAR 2010 criteria for RA. The degree of discordance was determined by descriptive statistics.
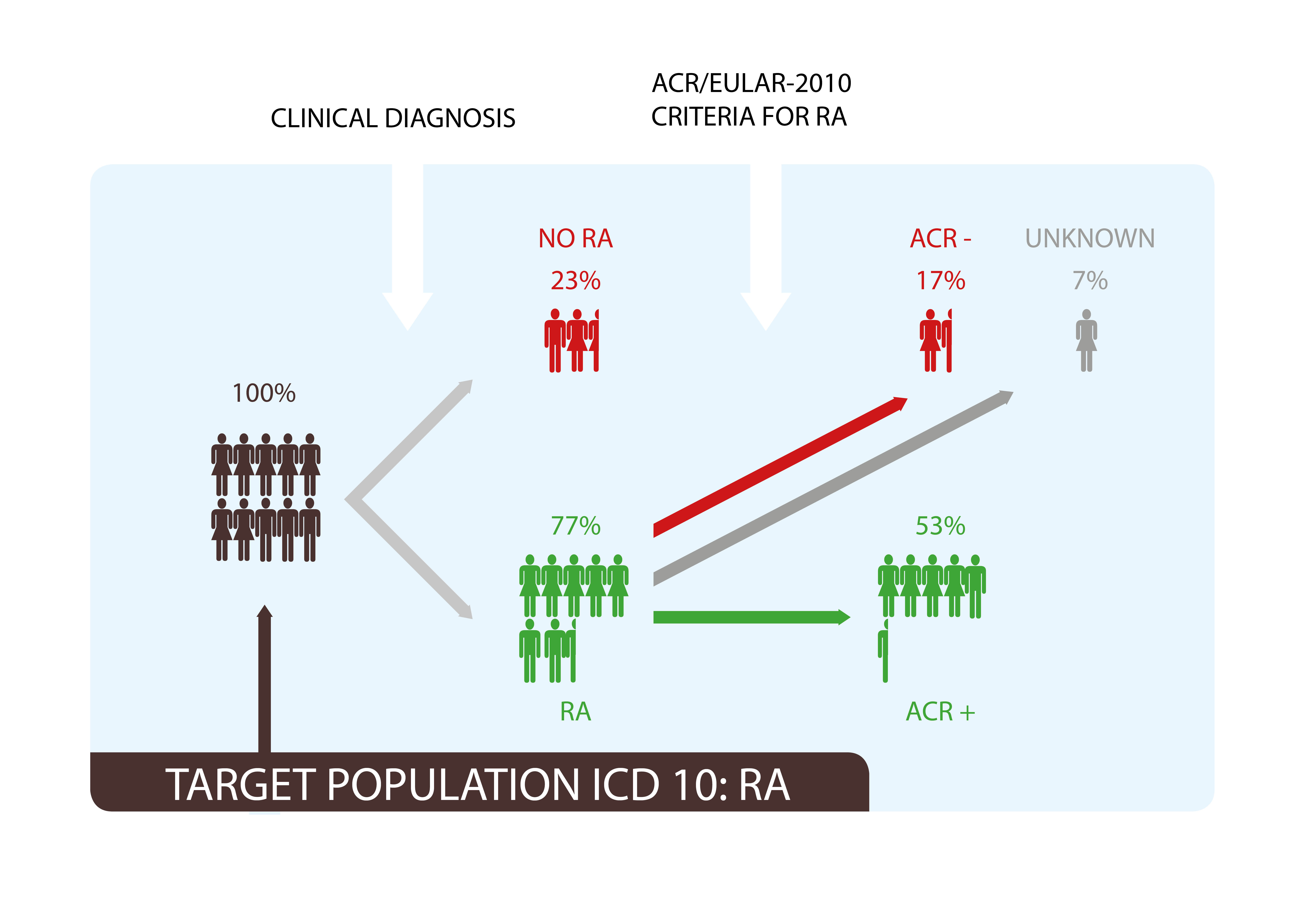
Results: A total number of 1641 patients were identified by DTC RA. The majority of the population was female (73%) with a mean age of 55 at time of RA diagnosis. According to the rheumatologist 371(23%) patients did not had RA. From the remaining 1270 patients who received the diagnosis RA according to the rheumatologist, 272(17%) did not fulfill the ACR/EULAR 2010 criteria (Figure 1). The patients who did not fulfill the ACR/EULAR 2010 criteria had less inflammation, were more often RF and/or ACPA negative, and had less involved joints, in terms of patient characteristics there was no significant difference within the groups. Approximately 10% of the data were missing at random.
Conclusion: For the measurement of healthcare quality and outcomes within a VBHC system, the patient population needs to be clearly defined and identified from hospital data sources. ICD-10 allows for baseline stratification. In this study we compared the financial DTC-RA registration, clinical diagnosis and ACR/EULAR classification criteria, and found a total discrepancy of 40%. Unfortunately from these descriptive analyses, it can be concluded that the ICD-10/DTC-RA codes are not the most reliable source of information on which the patient selection should be based. It is expected that this degree of misregistration for RA will have an impact on the value-based driven reimbursement system which we are currently investigating.
To cite this abstract in AMA style:
Conijn N, Lopes Barreto D, Kuijper M, van der Steen M, van der Kooij J, Weel A, Hazes JMW, Kok MR. the Impact of Diagnostic Misregistration of Rheumatoid Arthritis on the Establishment of a Value Based Healthcare System [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/the-impact-of-diagnostic-misregistration-of-rheumatoid-arthritis-on-the-establishment-of-a-value-based-healthcare-system/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-diagnostic-misregistration-of-rheumatoid-arthritis-on-the-establishment-of-a-value-based-healthcare-system/