Session Information
Date: Sunday, November 12, 2023
Title: (0543–0581) SLE – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with systemic lupus erythematosus (SLE) suffered from an increasing risk of cardiovascular diseases (23·3 events per 1000 patient-years). Antiphospholipid antibodies (aPLs), including anticardiolipin antibodies (aCL), anti-????2 glycoprotein I antibodies (aβ2GPI), and lupus anticoagulant (LA), increase the risk of thrombotic events in antiphospholipid syndrome, but the impact of aPLs on SLE patients was not yet determined. In this multi-center prospective study, we aimed to determine the association between aPLs and future atherosclerotic cardiovascular disease (ASCVD) risk in SLE.
Methods: Seven aPL isotypes (aCL IgG/IgM/IgA, aβ2GPI IgG/IgM/IgA, and LA) were measured based on international guidelines at SLE diagnosis and during follow-up. Clinical manifestations, disease activity status and organ damage were collected. Future ASCVD events were defined as new onset nonfatal myocardial infarction, nonfatal stroke, coronary or peripheral artery revascularization, or cardiovascular death.
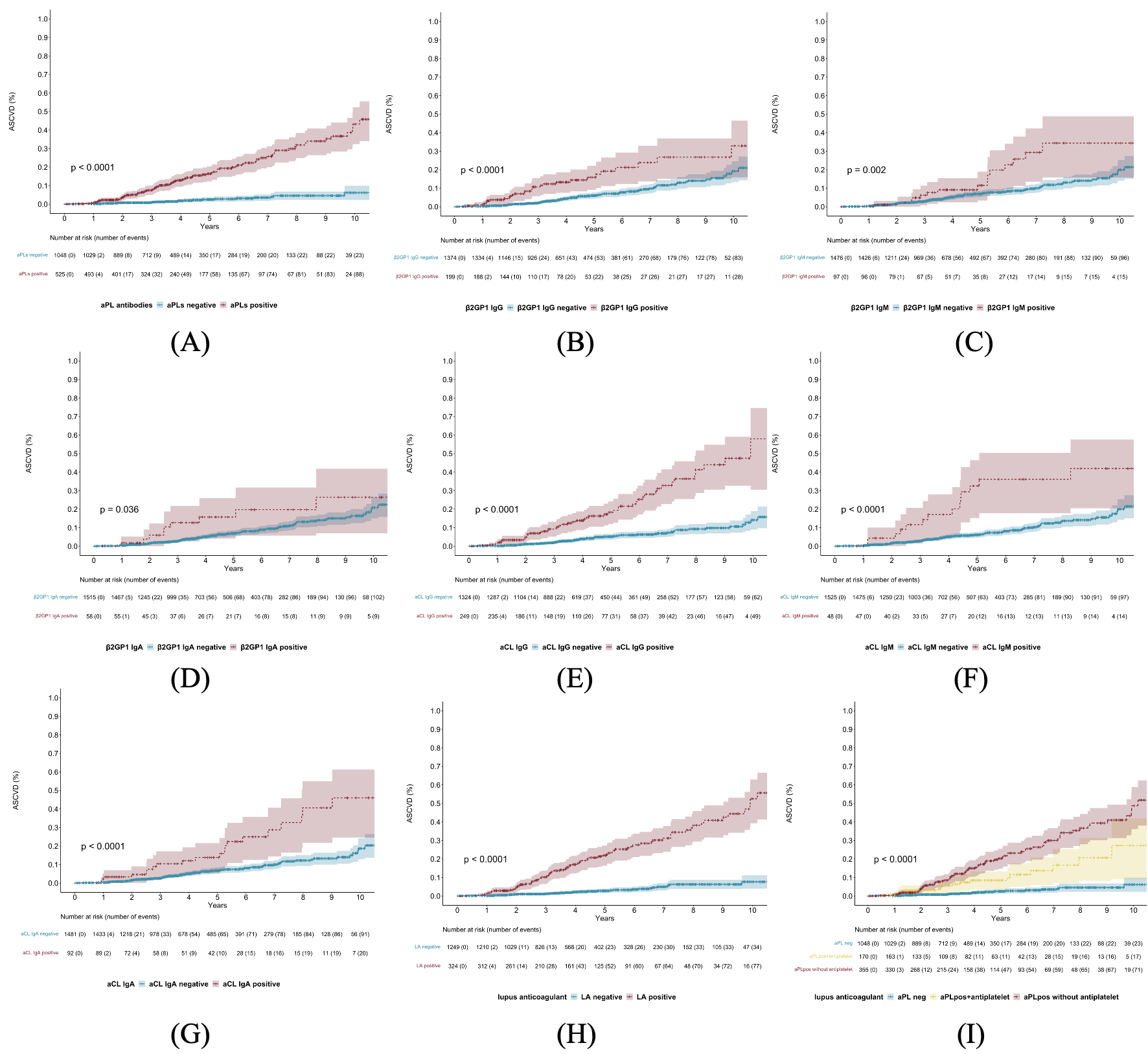
Results: Among the 1573 recruited SLE patients, 525 (33.4%) had positive aPLs. LA had the highest prevalence (324 [20.6%]), followed by aCL IgG (249 [15.8%]), aβ2GPI IgG (199 [12.7%]), aCL IgA (58 [3.7%]), aβ2GPI IgM (83 [5.3%]), aβ2GPI IgA (58 [3.7%]), aCL IgM (92 [5.8%]). 116 (7.37%) patients developed ASCVD during the mean follow-up of 4.51±2.32 years and 92 patients were aPLs positive. In univariate Cox regression analysis, both aPLs (HR=7.81, 95% CI, 5.00-12.24, p< 0.001) and traditional risk factors of cardiovascular disease were associated with future ASCVD events (Table 1). Kaplan-Meier plots suggested a potential trend towards ASCVD in positive versus negative aPLs antibodies. More importantly, anticoagulant or antiplatelet therapy can reduce ASCVD risk in SLE patients with positive aPLs (HR=0.57, 95% CI,0.25-0.93, P=0.026) (Figure 1). In multiple Cox regression analysis, aCL IgG (HR=1.95, 95% CI, 1.25-3.00, p=0.003), aCL IgM (HR=1.83, 95% CI, 1.03-3.20, p=0.039), and LA (HR=5.13, 95% CI 3.23-8.20, p< 0.001) positivity remained independently associated with ASCVD; traditional risk factors for ASCVD, including smoking, gender, age and hypertension, also play an independent role in SLE patients (Figure 2).
Conclusion: SLE patients with positive aPLs, especially positive aCL IgG/IgM and LA, warrant more care and surveillance of future ASCVD events during follow-up. Antithrombotic therapy has a protective effect on future ASCVD.
To cite this abstract in AMA style:
Ding Y, Huang C, zhao J, Wang Q, Tian X, Li M, Zeng x. The Impact of Antiphospholipid Antibodies on Future Atherosclerotic Cardiovascular Disease Risk in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/the-impact-of-antiphospholipid-antibodies-on-future-atherosclerotic-cardiovascular-disease-risk-in-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-antiphospholipid-antibodies-on-future-atherosclerotic-cardiovascular-disease-risk-in-systemic-lupus-erythematosus/