Session Information
Date: Tuesday, November 9, 2021
Title: RA – Treatments Poster III: RA Treatments & Their Safety (1674–1710)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Hydroxychloroquine (HCQ) has been used safely for over 60 years in rheumatic patients. However, following its recent use in covid-19 disease, its safety has been questioned, following controversial reports of cardiac toxicity, possibly related to a prolongation of the QT interval. Furthermore, it was recently shown that concomitant administration of different drugs can affect QT interval in hydroxychloroquine chronic users.
Methods: 12-lead electrocardiograms were recorded in 355 ambulatory patients (SLE = 85, RA = 80, SSc = 71, UCTD = 68, other CTDs = 51). The analysis was performed on corrected QT intervals (QTc) calculated according to Framingham formula (QTc = QT+0.154 (1−RR)), with ULN = 449 ms in males, and 467 ms in females. Glomerular filtrate rate (eGFR) was calculated with the CKD-EPI equation. The influence on QTc values of demographic variables, chronic (≥3 months) HCQ treatment, and of the use of 23 comedications -including corticosteroids, immunosuppressants, biologics, statins, aspirin, angiotensin converting enzyme inhibitors, angiotensin receptor blockers, diuretics, betablockers, endothelin antagonists, duloxetine, selective serotonin reuptake inhibitors, gabapentinoids, proton-pump inhibitors (PPI), calcium channel blockers (CCBs) – were evaluated by parametric or non parametric statistical methods, as appropriate. All statistic analyses were performed with the IBM SPSS statistical package version 25.
Results: Demographic variables, and the use of comedications were not different in HCQ+ and HCQ- patients (Table 1). In the whole population, the QTc mean duration was 416.44 ± 19.53 ms, and was correlated with age (Fig. 1; r = 0.211, p < 0.001), but not with gender (F: 417.79±19.02 ms, M: 413.21±23.73 ms, p = 0.303), eGFR (r = -0.83, p = 0.120), BMI (-0.001, p = 0.984) or disease (p = 0.139). In only 4 patients (HCQ+: 3 (1.5%) – HCQ-: 1 (0.6%), p = 0.629) QTc duration was above ULN.
The patients were heavily cotreated, with 5.64 ± 3.47 concomitant medications on average (HCQ+ 5.58±3.47; HCQ- 5.59±3.33, p=0.804). Among the 23 cotreatments evaluated in univariate analyses, QTc duration was associated only with the assumption of vitamin D (418.95±19.56 ms vs 411.38±18.53 ms, p = 0.001), PPIs (419.14±20.00 ms vs 412.89±16.86 ms, p = 0.003), and CCBs (421.61±24.41 ms vs 415.53±18.44 ms, p = 0.036). In the analysis of covariance on age-adjusted data, only HCQ (p < 0.001) and Vitamin D (p =0.046) but not PPIs (p = 0.121) nor CCBs (p = 0.200) were still significantly correlated to QTc interval. Furthermore, as reported in Fig. 2, our data show a trend - albeit not statistically significant - towards an additive effect on QT prolongation of the association of Vitamin D, PPIs and CCBs with HCQ, even more evident in the case of association of the 3 drug classes.
Conclusion: In this study, the QTc interval duration was correlated to age and was significantly prolonged in patients treated with hydroxychloroquine as compared to controls, although significant prolongation was extremely infrequent. Furthermore, our data revealed signs of drug-drug interference, suggesting that regular monitoring of the electrocardiogram is advisable in these patients, often undergoing cotreatment with multiple drugs.
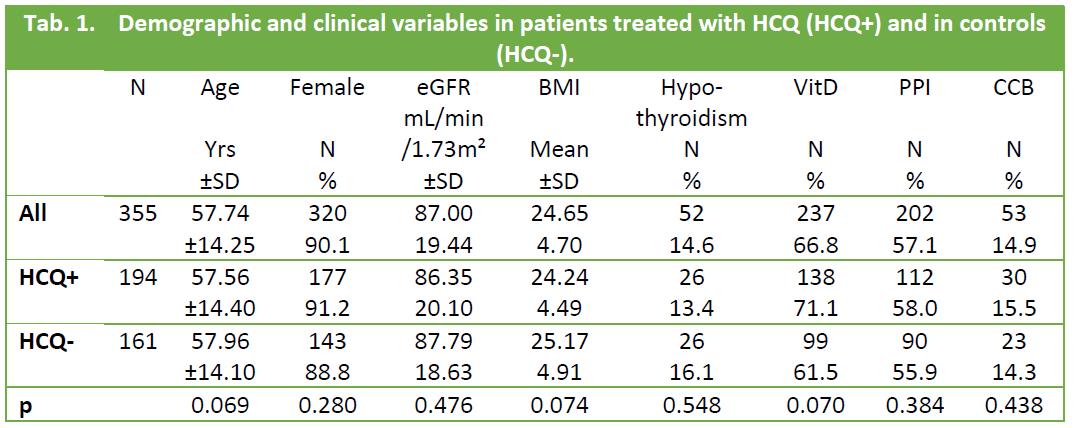 Tab. 1. Demographic and clinical variables in patients treated with HCQ (HCQ+) and in controls (HCQ-).
Tab. 1. Demographic and clinical variables in patients treated with HCQ (HCQ+) and in controls (HCQ-).
 Fig 1. Correlstion between age and Qtc interval
Fig 1. Correlstion between age and Qtc interval
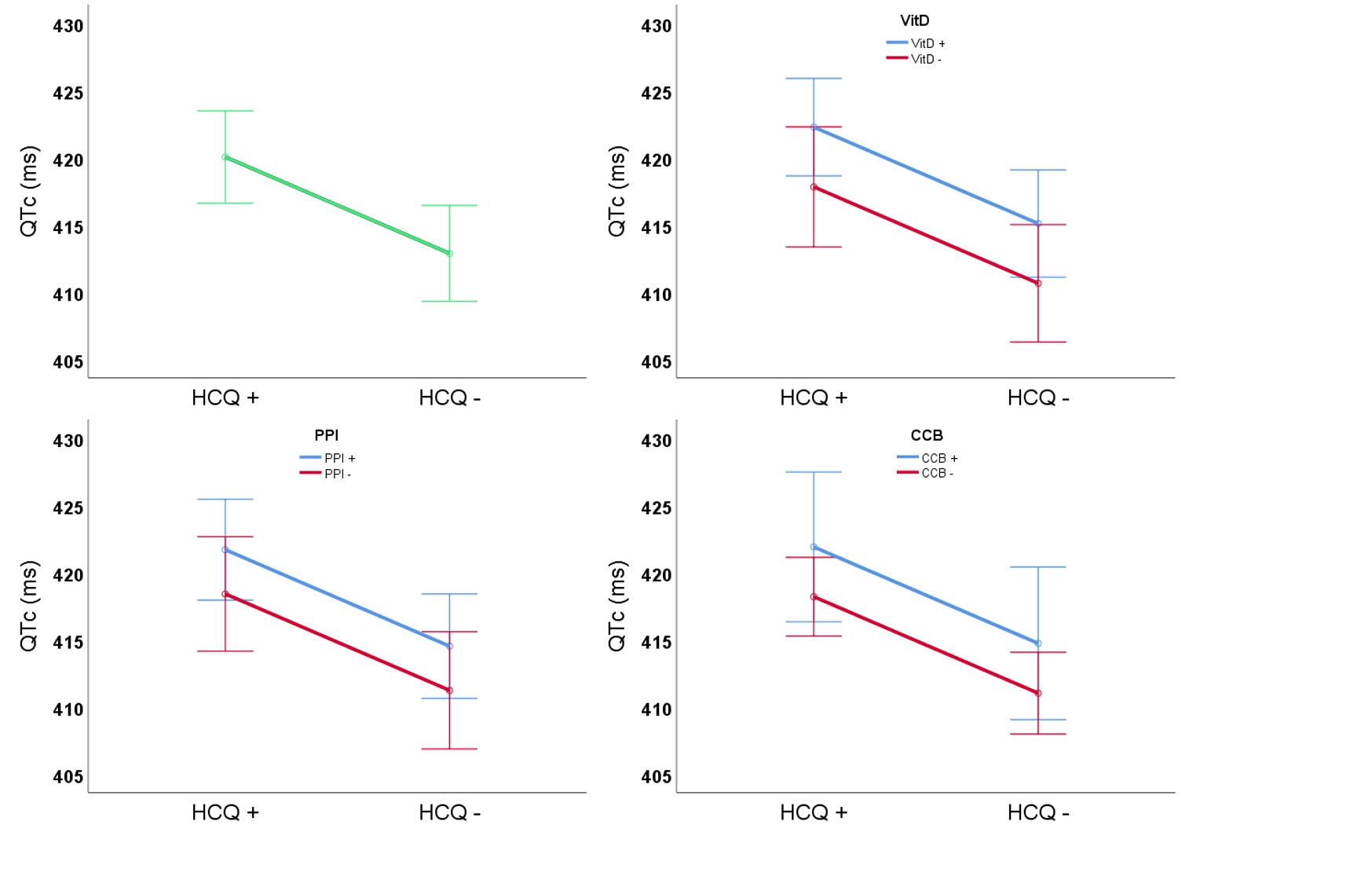 Fig. 2. Influence of selected cotreatments in patients treated with HCQ and in controls
Fig. 2. Influence of selected cotreatments in patients treated with HCQ and in controls
To cite this abstract in AMA style:
Antivalle M, Agosti M, La Paglia G, Batticciotto A, Ditto M, PARISI S, Sarzi-Puttini P. The Impact of Age and Drug-Drug Interactions on QT Interval in Chronic Hydroxychloroquine Users [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/the-impact-of-age-and-drug-drug-interactions-on-qt-interval-in-chronic-hydroxychloroquine-users/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-age-and-drug-drug-interactions-on-qt-interval-in-chronic-hydroxychloroquine-users/
