Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: The aim of this study was to assess the immune, growth and development characteristics in offspring born to mothers with systemic lupus erythematosus (SLE).
Methods: Children who were born in Peking University People’s Hospital from May 2008 to November 2021 were followed up. The antibody profile, immune cell subsets were tested. A face-to-face evaluation of growth and development were done by a pediatrician. The laboratory tests of mothers with systemic lupus erythematosus were collected before, during, and after delivery.
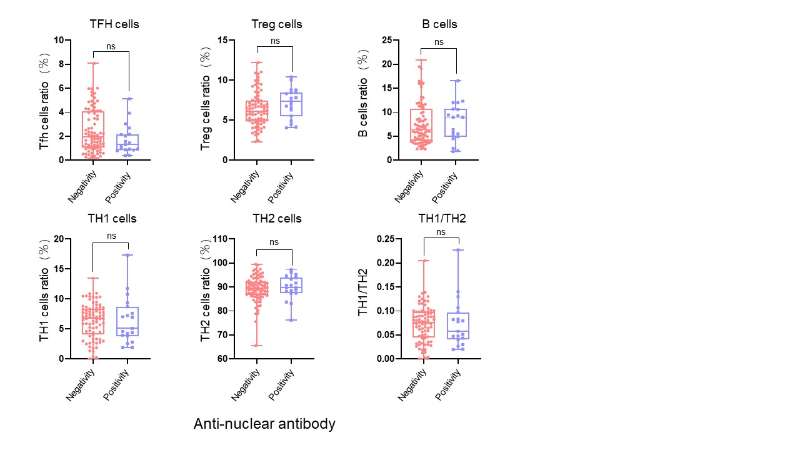
Results: Ninety-nine children were born to 78 SLE mothers. There were 47 (47.47%) boys and 52 (52.52%) girls. The age of children was 6.63±2.59 years. Twenty-five (25.25%) children had positive anti-nuclear antibody (ANA) at birth, and 19 (19.19%) children had persistently positive ANA. Children who had neonatal lupus (1.25% vs. 15.79%, P=0.022) present higher incidence of persistently positive ANA. However, there were no differences in neonatal pathological jaundice (17.50% vs. 21.05%, P=0.976), infectious diseases (26.25% vs. 47.37%, P=0.072), allergic diseases (48.75% vs. 52.63%, P=0.761), nutritional metabolic diseases (1.25% vs. 5.26%, P=0.349), long-term growth retardation (7.50% vs. 5.26%, P=1.000), and long-term neurodevelopment (Conners Index of Hyperactivity) (3.75% vs. 0.00%, P=1.000) between children with negative ANA and persistently positive ANA. Except for the increase of ANA positive rate (36.00% vs. 10.87%, P=0.004) at birth, there were no significant differences in neonatal lupus (4.00% vs. 4.35%, P=1.000), infectious diseases (28.00% vs. 32.61%, P=0.623), allergic diseases (54.00% vs. 47.83%, P=0.545), nutritional metabolic diseases (0.00% vs. 4.35%, P=0.227), long-term growth retardation (10.00% vs. 4.35%, P=0.502), and long-term neurodevelopment (4.00% vs. 2.17%, P=1.000) between mothers who took or didn’t take glucocorticoid during pregnancy. The same results were found for the use of hydroxychloroquine during pregnancy. No statistically differences were found in immune cells between persistently ANA-positive and ANA-negative children, including Tfh cells (P=0.013), Treg cells (P=0.092), B cells (P=0.625), TH1 cells (P=0.660), TH2 cells (P=0.525) and TH1/TH2 (P=0.619). Univariate logistic regression analysis showed that neonatal lupus (OR=14.812, 95%CI: 1.447~151.647, P=0.023) was a risk factor for persistently positive ANA.
Conclusion: Neonatal lupus is a risk factor for persistently positive ANA. However, persistently positive ANA does not increase the risk of infectious diseases, allergic diseases, nutritional metabolic diseases, growth retardation, neurodevelopmental abnormality, and immune cells abnormalities in the offspring with SLE mothers.
To cite this abstract in AMA style:
Wang W, Hu X, Wang H, Yu S, Xie M, Shao S, Li c, He J. The Immune and Growth Characteristics of Children Born to Mothers with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/the-immune-and-growth-characteristics-of-children-born-to-mothers-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-immune-and-growth-characteristics-of-children-born-to-mothers-with-systemic-lupus-erythematosus/