Session Information
Date: Sunday, November 13, 2022
Title: SLE – Diagnosis, Manifestations, and Outcomes Poster II: Manifestations
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Immune thrombocytopenic purpura (ITP) is an organ-specific autoimmune disease and its etiopathogenetic mechanisms are suggestive of systemic autoimmune diseases (SAD) such as systemic lupus erythematosus (SLE). Thrombocytopenia is also frequently present in SLE patients and has been associated with poor prognosis. Recent population-based cohort studies suggest that the incidence of SLE is increased in ITP patients and that isolated ITP with a positive Anti-nuclear antibody (ANA) may be at much higher risk of developing SAD. In this study, we performed a meta-analysis to evaluate the development of SLE in patients with ITP.
Methods: Literature search was performed by using terms ‘immune thrombocytopenia’, ‘antinuclear antibody’ and ‘systemic lupus erythematosus’ in PubMed, Web of Science and Cochrane Library without any restrictions prior to May 2022. Studies were included that reported development of SLE in ITP patients. Forest plot was used to detect overall SLE frequency in ITP and compare risk ratios for SLE development in different ITP subgroups. In addition, we also evaluated childhood-onset (≤16 years).
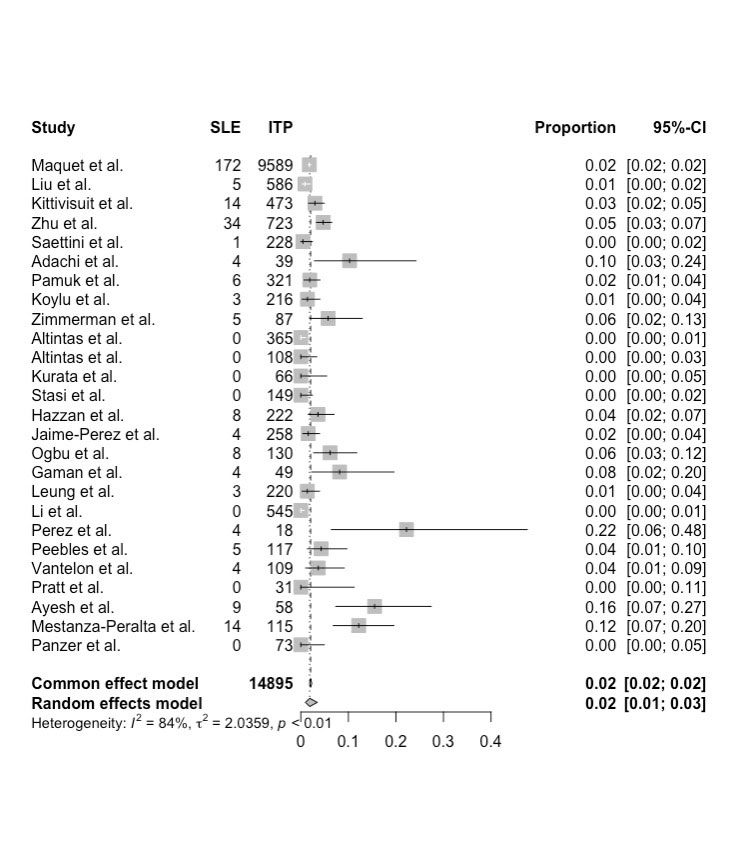
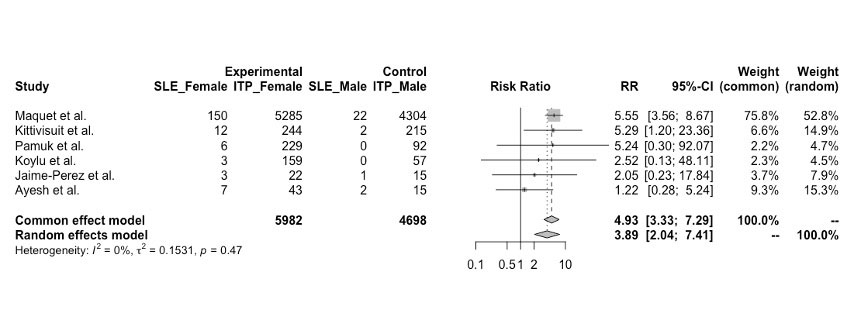
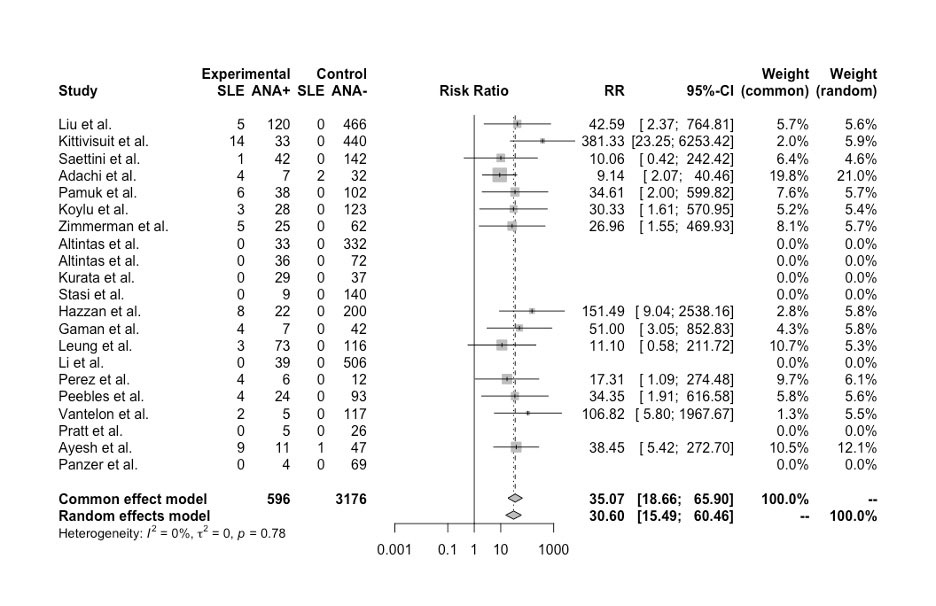
Results: 26 eligible studies comprising 14895 ITP patients were included in analysis. 307 ITP patients developed SLE during the follow-up period (range: 1.1- 14 years) (2.06%, 95%CI: 1.8-2.3%) (Figure 1). The rates of SLE in aITP and cITP cases were not significantly different, 2.02% (95%CI: 1-4%) and 2.4 (95%CI: 1.7-3.3%) respectively. Relative risk (RR) for developing SLE was significantly higher in female ITP patients (RR: 4.93, 95%CI: 3.33-7.29, p< 0.001) (Figure 2). ANA was reported in 21 studies that included 3772 ITP patients (3176 ANA negative ITP, 596 ANA positive ITP {15.5%}). There was significantly increased risk of SLE development (RR: 35.07, 95%CI: 18.66-65.9, p< 0.001) in ANA positive patients (Figure 3). cITP patients had higher RR for SLE development than aITP patients, however, the difference was not significant (RR-cITP: 74.93, 95%CI: 22.83-245.99, RR-aITP: 25.56 (95%CI: 11.76-55.49).
Conclusion: We identified ITP patients at higher risk of developing SLE in future. Pooled data revealed that positive ANA (present in 15.5%) and females are at significantly higher risk of developing SLE. Although the difference was not statistically significant, but SLE was more common in cITP patients.
To cite this abstract in AMA style:
Pamuk O, Hasni S. The Frequency of Systemic Lupus Erythematosus in Patients with Immune Thrombocytopenic Purpura: A Systematic Meta-analysis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/the-frequency-of-systemic-lupus-erythematosus-in-patients-with-immune-thrombocytopenic-purpura-a-systematic-meta-analysis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-frequency-of-systemic-lupus-erythematosus-in-patients-with-immune-thrombocytopenic-purpura-a-systematic-meta-analysis/