Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
Elderly patients with ANCA associated vasculitides (AAV) seem to have clinical differences compared to younger patients. The aim of this study is to compare clinical and laboratory characteristics, survival and mortality rates of patients with AAV with respect to age at diagnosis.
Methods:
Medical records of patients with microscopic polyangiitis (MPA), granulomatosis with polyangiitis (GPA) or eosinophilic granulomatosis with polyangiitis (EGPA), classified according to the European Medicine Agency classification algorithm and followed up by Ege University Hospital Rheumatology Department between 1997 and 2017 were retrospectively analyzed. Patients were divided into two groups based upon age at disease onset: <65 years (Group 1) and ≥65 years (Group 2). Gender, age at diagnosis, time to diagnosis, follow up time, involved organs/systems, pattern of ANCA positivity, type of AAV and number of deaths were noted. Chi-square test, two-way t test, cox regression analysis and Kaplan-Meier method were used to compare the groups.
Results:
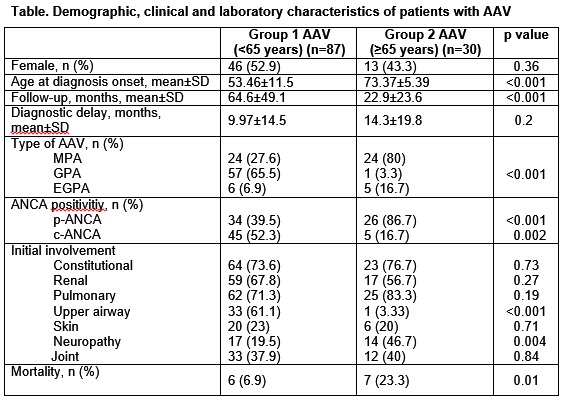
In our cohort, 87 patients <65 years and 30 patients ≥65 years were enrolled. Demographic, clinical and laboratory characteristics of those patients are given in Table. There were no differences in gender and smoking status between the groups, but the rates of malignancy, hypertension and hyperlipidemia were higher in Group 2. Upper airway involvement was more frequent in Group 1, peripheral neuropathy was more frequent in Group 2. These findings were probably due to more frequent occurrence of GPA in Group 1 and MPA in Group 2.
As expected, mortality rate was higher in Group 2 (Table). The mean survival time was 221 ± 7.47 months for Group 1, and 65 ± 8.14 months for Group 2. One-year, 2-years, 5-years and 10-years survival rates were 96%, 96%, 91%, and 91% in Group 1, respectively. On the other hand, one-year, 2-years and 5-years survival rates were 81%, 70% and 70% for group 2, respectively. Ten-years survival rates could not calculated for Group 2. One death (1/6) in Group 1 and six deaths (6/7) in Group 2 were due to opportunistic infections.
Being diagnosed at the age of 65 years or over increased the mortality by 48.7 times compared to being diagnosed before the age of 65 years (%95 CI: 6.37-372.09, p<0,001). We also found out that each increase of one year at the age of diagnosis resulted in an increment in the mortality 1.1 times (%95 CI:1,03-1,18, p:0,003). When age factor is removed, type of AAV, basal serum creatinine level and having GFR <50 ml/min per 1.73 m2 did not affect the mortality significantly.
Conclusion:
In our study, the age at diagnosis was established to be the most significant factor on mortality of AAV. We found out that basal serum creatinine level and GFR did not affect the mortality critically, when adjusted by age. Because of the high mortality rate, more attention should be paid to the management of AAV patients diagnosed at advanced age.
To cite this abstract in AMA style:
Kara M, Taş MN, Durusoy R, Ketenci S, Pekdiker M, Öz HE, Aşçı G, Keser G, Aksu K. The Effect of Age at Diagnosis on Mortality in ANCA-Associated Vasculitides [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/the-effect-of-age-at-diagnosis-on-mortality-in-anca-associated-vasculitides/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-effect-of-age-at-diagnosis-on-mortality-in-anca-associated-vasculitides/