Session Information
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: African Americans (AA) are more likely to experience psychosocial and environmental stressors and develop SLE than whites. Increasing frequency of racial discrimination is associated with greater damage in SLE. Cardiovascular disease (CVD) is a leading cause of SLE morbidity and mortality. However, the increased CVD risk is not completely attributable to SLE activity and traditional CVD risk factors. We examined whether discrimination affects CVD risk after taking stress into account in patients with SLE.
Methods: The Georgians Organized Against Lupus (GOAL) is a population-based cohort of validated SLE patients in Atlanta derived from the Centers for Disease Control and Prevention supported Georgia Lupus Registry who consent to complete annual surveys across multiple domains. We analyzed 2 validated measures of psychosocial stress, Perceived Stress Scale (PSS) and Everyday Discrimination Scale (EDS), in the 2017 survey. Potential CVD events (ever) through 2016 were identified by patient report and by Georgia Hospital Discharge Database CVD-related codes. Medical records were reviewed by study physicians. CVD events (myocardial infarction, angina, transient ischemic attack, stroke, and/or peripheral vascular disease) were adjudicated using validated algorithms. Logistic regression was used to separately explore the association between PSS and CVD and EDS and CVD in univariate and multivariate analyses.
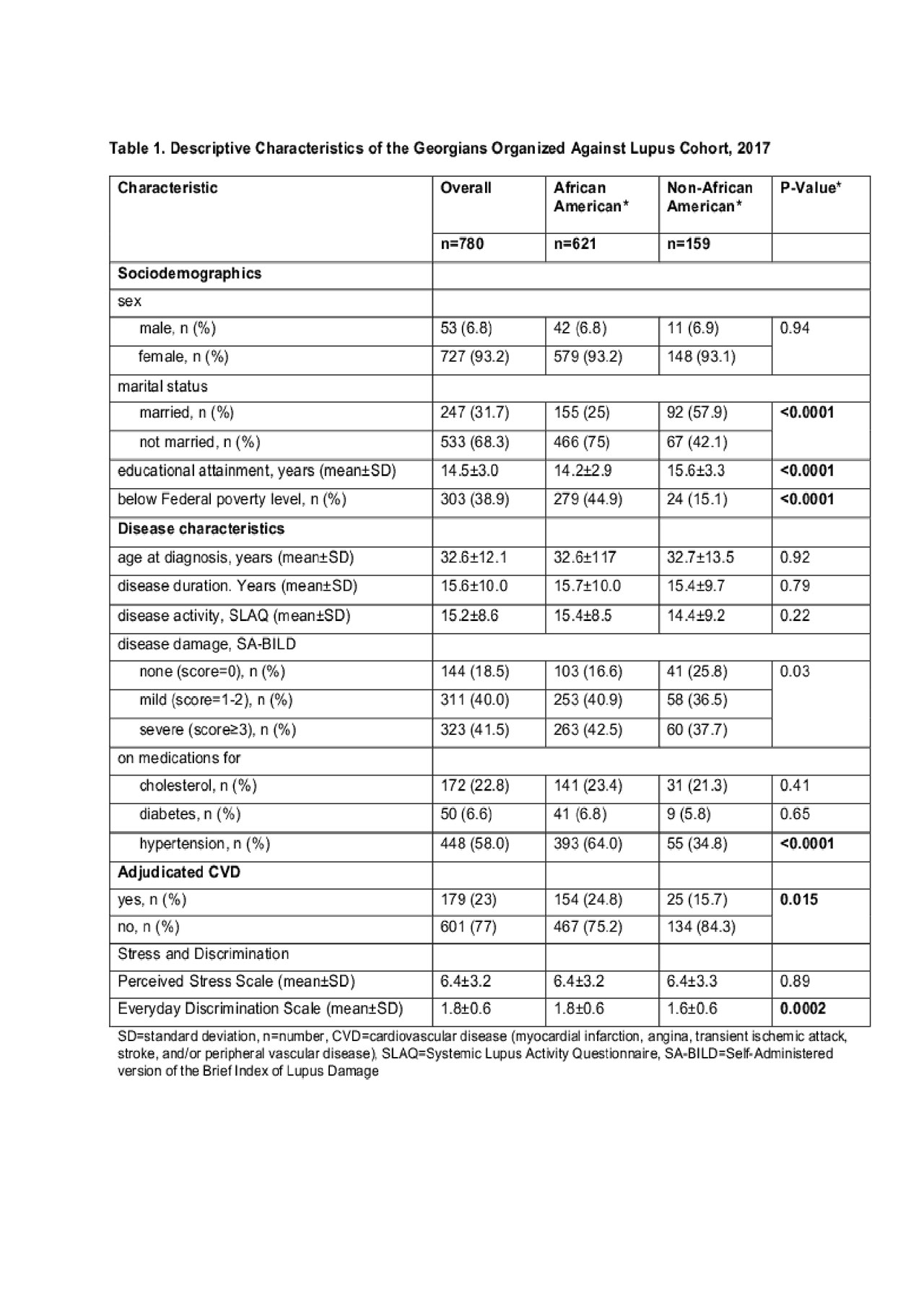
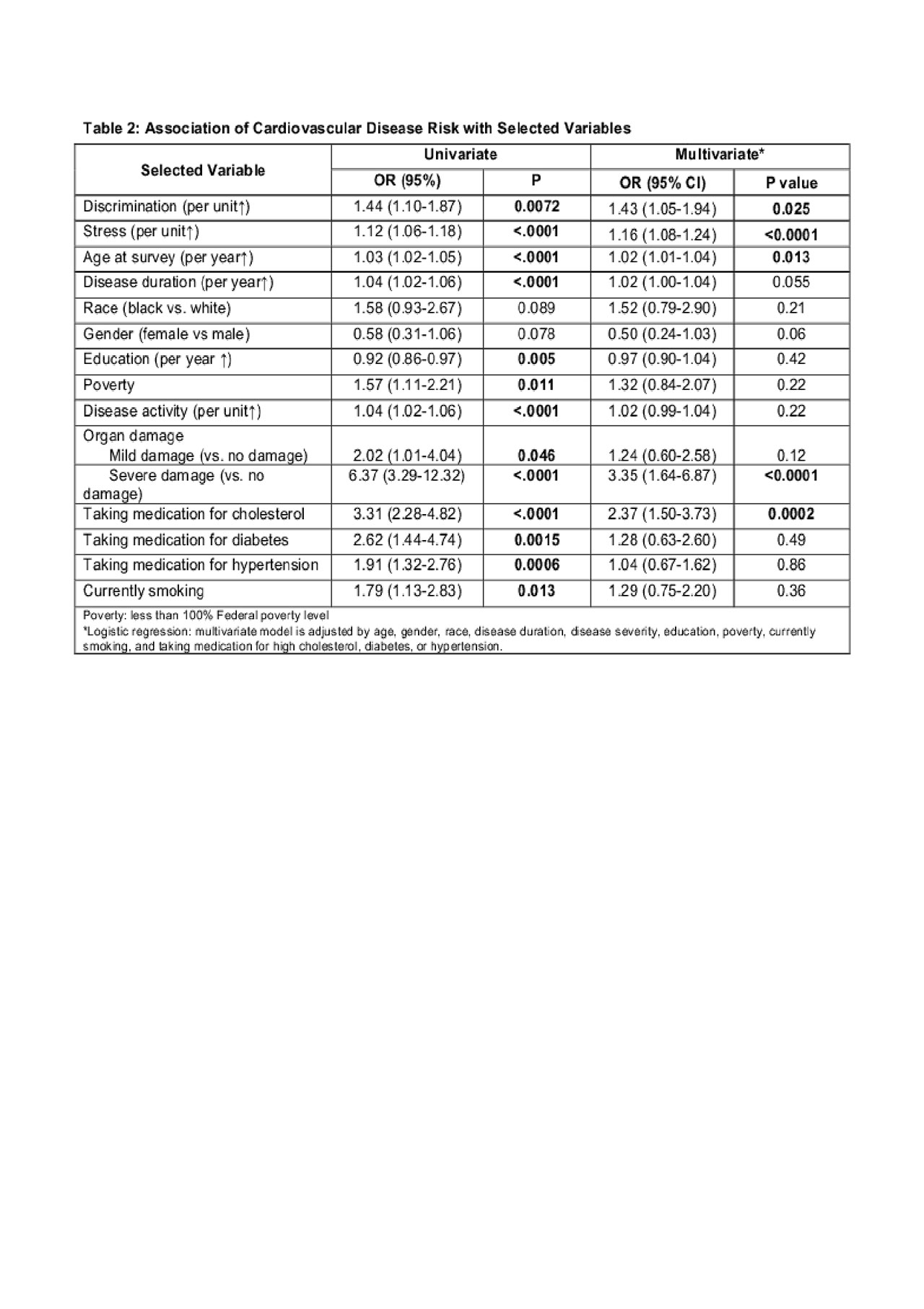
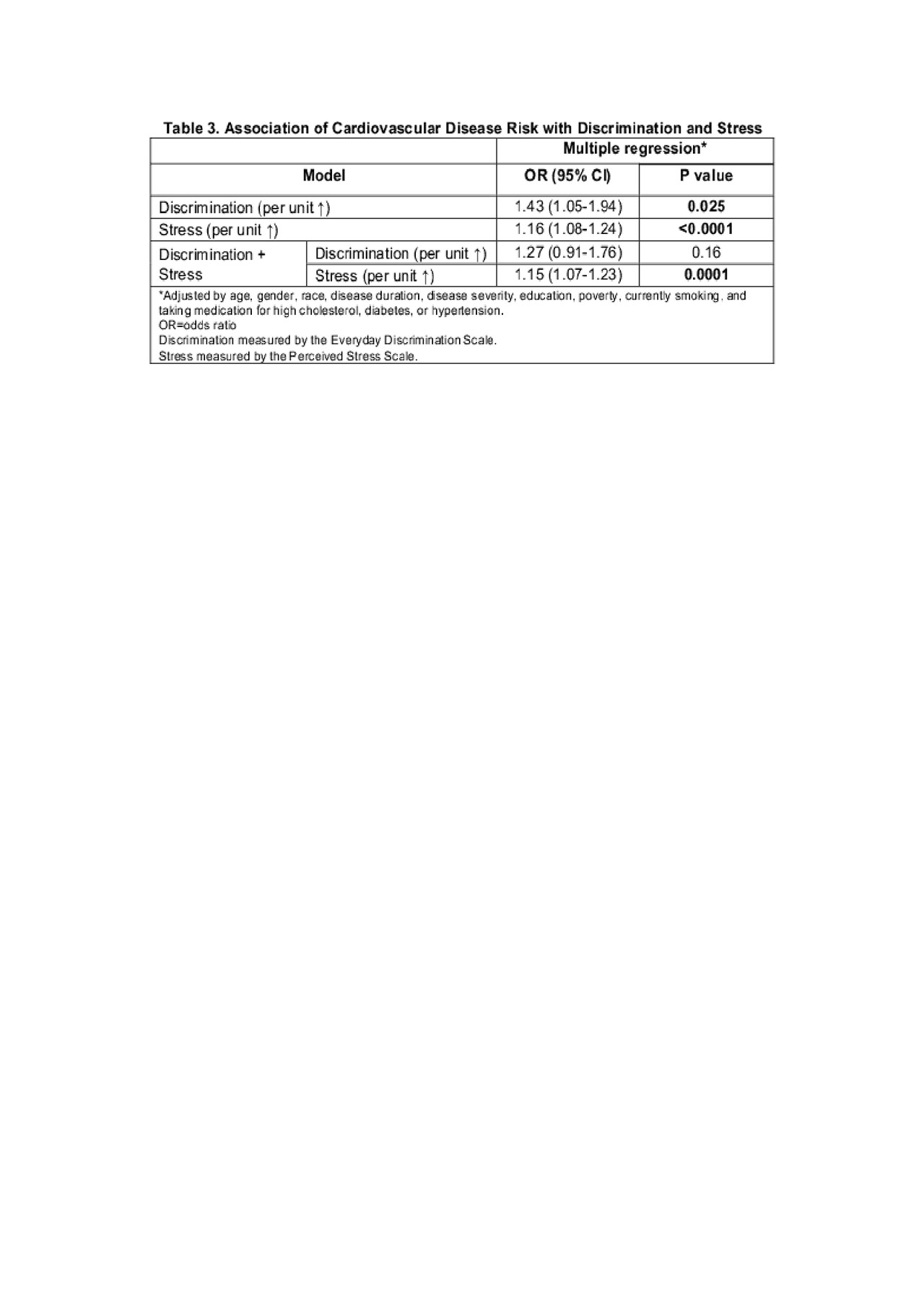
Results: The 2017 GOAL survey was comprised of 780 patients, of whom 621 (79.6%) were AA, 110 (14.1%) were white, and 49 (6.3%) from other racial/ethnic groups. A total of 179 (23%) patients were adjudicated as having had CVD. AA’s had more CVD (24.8% vs. 15.7%, p=0.015), reported higher EDS score (1.8 vs 1.6, P=0.0002), but no difference in PSS level (6.4 vs 6.4, p=0.89) compared with non-AA’s (Table 1). Multivariate logistic regression analysis demonstrated a significant association between both EDS and PSS with CVD after controlling for race; age; gender; SLE activity, damage, and duration; being on medications for cholesterol, diabetes, and hypertension; currently smoking; and poverty (Table 2). The significance of the association was no longer present after including PSS in the model (Table 3).
Conclusion: Including PSS in the model of discrimination and CVD no longer made the association significant, suggesting the association between discrimination and CVD is principally through high stress levels. High stress is known to contribute to the development of atherosclerosis in the general population. In those with SLE, discrimination may result in greater CVD risk through higher stress rather than a result of being a certain race. In our study, the burden of psychosocial stress was higher in AA’s than non-AA’s, which may explain, in part, racial disparities in past CVD events along with poorer control of CVD risk factors. Including social determinants of health in the lupus health disparities framework provides a more comprehensive understanding of why low-income communities and communities of color experience poorer outcomes. Further research into related causal pathways, mitigating factors, and biologic mechanisms is also needed.
To cite this abstract in AMA style:
Lim S, Bao G, Helmick C, Dunlop-Thomas C, Drenkard C. The Association of Discrimination and Stress on Cardiovascular Disease in a Population-Based Cohort with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-association-of-discrimination-and-stress-on-cardiovascular-disease-in-a-population-based-cohort-with-systemic-lupus-erythematosus/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-association-of-discrimination-and-stress-on-cardiovascular-disease-in-a-population-based-cohort-with-systemic-lupus-erythematosus/