Session Information
Date: Tuesday, November 12, 2019
Title: Vasculitis – Non-ANCA-Associated & Related Disorders Poster III: Giant Cell Arteritis
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Bisphosphonates have been used to treat disorders of bone metabolism for several years. A common adverse reaction associated with their use constitutes a transient acute-phase response mediated by increased pro-inflammatory cytokine release. This can affect up to 40% of patients and is characterized by fever, joint swelling, and orbit inflammation. GCA is a condition characterized by granulomatous inflammation involving medium-to-large sized arteries. Pro-inflammatory cytokines are known to play a significant role in its pathogenesis. A case report linking the development of GCA with bisphosphonate use was recently published. We sought to describe the prevalence of GCA after bisphosphonate administration to further explore this possible relationship.
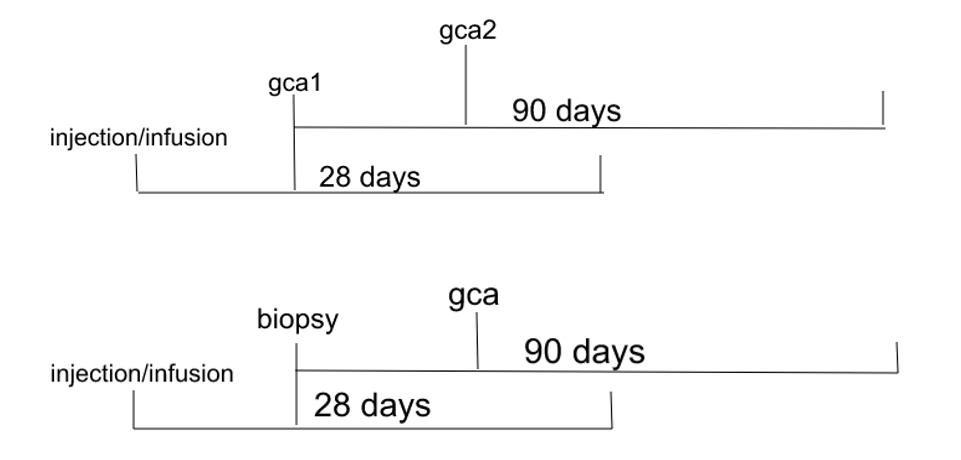
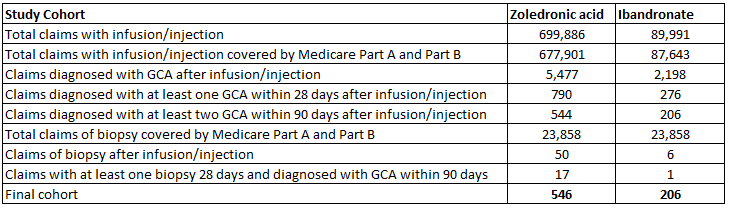
Methods: We used the 20% Medicare random sample data (including Part A and Part B) from between 2008 and 2014 to identify elderly patients who received either zoledronate or ibandronate infusions and subsequently developed GCA. We used two ways to identify such patients. In the first method we included patients who had the diagnosis of GCA claimed within 28 days of the infusion and again within 90 days of the initial diagnosis. In the second method we included patients who had a temporal artery biopsy performed within 28 days of the infusion and subsequently had a GCA diagnosis claimed within 90 days of their biopsy being performed. ICD-9-CM diagnosis codes were used to define diagnosis claims and Healthcare Common Procedure Coding System (HCPCS) code was used to identify the biopsy claim.
Results: We identified 677,901 claims for zoledronate and 87,643 for ibandronate out of which 546 and 206 respectively met our criteria for a diagnosis of GCA. Hence, the prevalence of GCA was 0.08% and 0.24% after zoledronate and ibandronate administration respectively. The prevalence of GCA was highest in the 75-85 years old age group with 0.1% for zoledronate and 0.3% acid for ibandronate. We found the prevalence to be higher in females compared to males for zoledronate (0.11% vs 0.03%) as well as for ibandronate (0.24% vs 0.2%). Racially, Hispanics compared to other races had the highest prevalence after zoledronate administration (0.11%), while Caucasians had the highest prevalence for ibandronate (0.25%). Looking at the regional level the highest prevalence was in the northeast for zoledronate (0.1%) and west for ibandronate (0.33%).
Conclusion: Clinicians should be cognizant that there could be an association between bisphosphonate therapy and the subsequent development of autoimmune reactions including GCA. This association may not follow the trend of preference for the Caucasian and Midwest populations as previously described. Further studies are needed to better elucidate this relationship and describe if differences exist in the incidence of GCA after treatment with different bisphosphonate therapies.
To cite this abstract in AMA style:
Mahmood S, Ji Y, Peng Y, Abou Zahr Z. The Association Between Bisphosphonates and Giant Cell Arteritis: A Retrospective Cohort Study [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-association-between-bisphosphonates-and-giant-cell-arteritis-a-retrospective-cohort-study/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-association-between-bisphosphonates-and-giant-cell-arteritis-a-retrospective-cohort-study/