Session Information
Date: Tuesday, November 7, 2017
Title: Health Services Research I: Cost Drivers in Rheumatic Disease
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Depression is significantly more prevalent in patients with rheumatoid arthritis (RA) compared with the general population.1 It has a significant effect on RA patients, compromising clinical outcomes and increasing mortality. The objective of this study is to compare the healthcare utilization, expenditures, and work productivity among patients with RA to patients with RA and depression.
Methods: The Truven Health MarketScan® Research Databases were used in the analysis. Patients ≥18 years of age with at least 2 RA visits, at least 2 months apart, between January 1, 2013 and December 31, 2013 were eligible for inclusion. The date of the first observed claim with an RA diagnosis was defined as the “index date.” Depression was defined as at least 2 visits for depressive disorder, at least 14 days apart, during the 12-month pre-index period in eligible patients. Outcomes were measured during the 12-month post-index period. Propensity score was calculated and controlled in logistics regression or Poisson regression. The incremental adjusted annual cost and 95% confidence interval (CI) were calculated using the bootstrapping method.
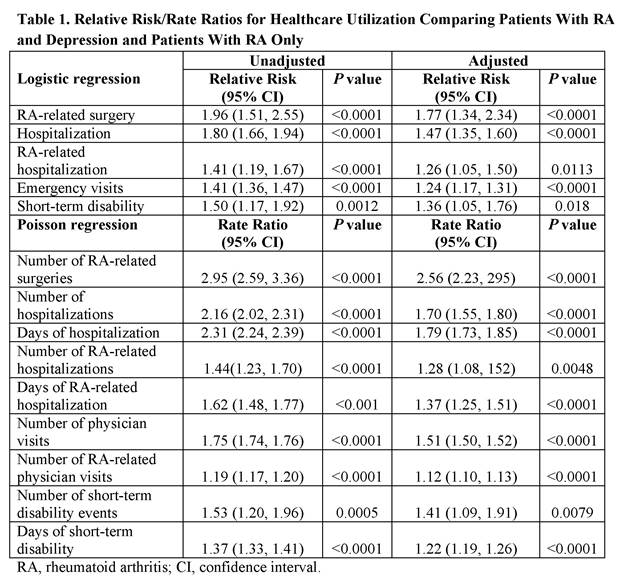
Results: A total of 46,700 RA patients were eligible for the analysis. Of this sample, 3,478 (7%) patients had RA and depression. The mean age of the study sample was 52 (standard deviation = 9.7) years and 78% were female. Patients with and without depression were significantly different (P <0.05) in terms of age, gender, residence area, relationship to primary insured, joint aspirations/injections, extra-articular manifestations, and difficulty walking, and had a wide variety of heterogeneous comorbidities at baseline. These covariates were used to calculate propensity score. After adjustment for propensity score, RA patients with depression used more healthcare resources annually compared with those without depression (relative risk and rate ratio >1 with P <0.05 for all outcomes in Table 1). The incremental adjusted annual direct cost was $8,488 (95% CI, $6,793-$10,223); while the RA-related incremental adjusted annual direct cost was $578 (95% CI, $-98-$1,243).
Conclusion: This study highlights economic burden due to the presence of depression in RA patients. These findings underline the importance of managing RA when treatment algorithms are devised for these patients.
Reference: 1Matcham F, et al. Rheumatology (Oxford). 2013;52(12):2136-2148.
To cite this abstract in AMA style:
Li N, Peterson S. The Additional Economic Burden of Depression Among Adults with Rheumatoid Arthritis in the United States [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/the-additional-economic-burden-of-depression-among-adults-with-rheumatoid-arthritis-in-the-united-states/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-additional-economic-burden-of-depression-among-adults-with-rheumatoid-arthritis-in-the-united-states/