Session Information
Date: Sunday, November 10, 2019
Title: Measures Of Healthcare Quality Poster I: Testing, Screening, & Treating
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: The ACR’s Rheumatology Informatics System for Effectiveness (RISE) is an EHR‐enabled registry that represents over 36% of the U.S. clinical rheumatology workforce and calculates patient-level performance on over 24 quality measures. RISE allows rheumatologists to track their performance on quality measures, but aggregate trends in performance have not been studied. The objectives of our study were to examine changes in performance over time on selected quality measures in patients with RA and assess variations in performance across practices.
Methods: We analyzed data from practices enrolled in RISE between January 1, 2015 and December 31, 2017. Eight quality measures in the areas of RA management (disease activity assessment, functional status assessment, DMARD prescribing, and tuberculosis (TB) screening), and risk reduction (tobacco use screening and cessation, blood pressure (BP) control, and two measures on high risk medication use in elderly) were examined. Practice-level performance was defined as the percentage of eligible patients receiving recommended care for each measure separately. We used hierarchical multivariate linear models to predict change in performance as a function of practice type (single-specialty group practice, multi-specialty group practice, solo practitioner vs. health system), after adjusting for patient demographics, number of providers, EHR vendor and geographic region.
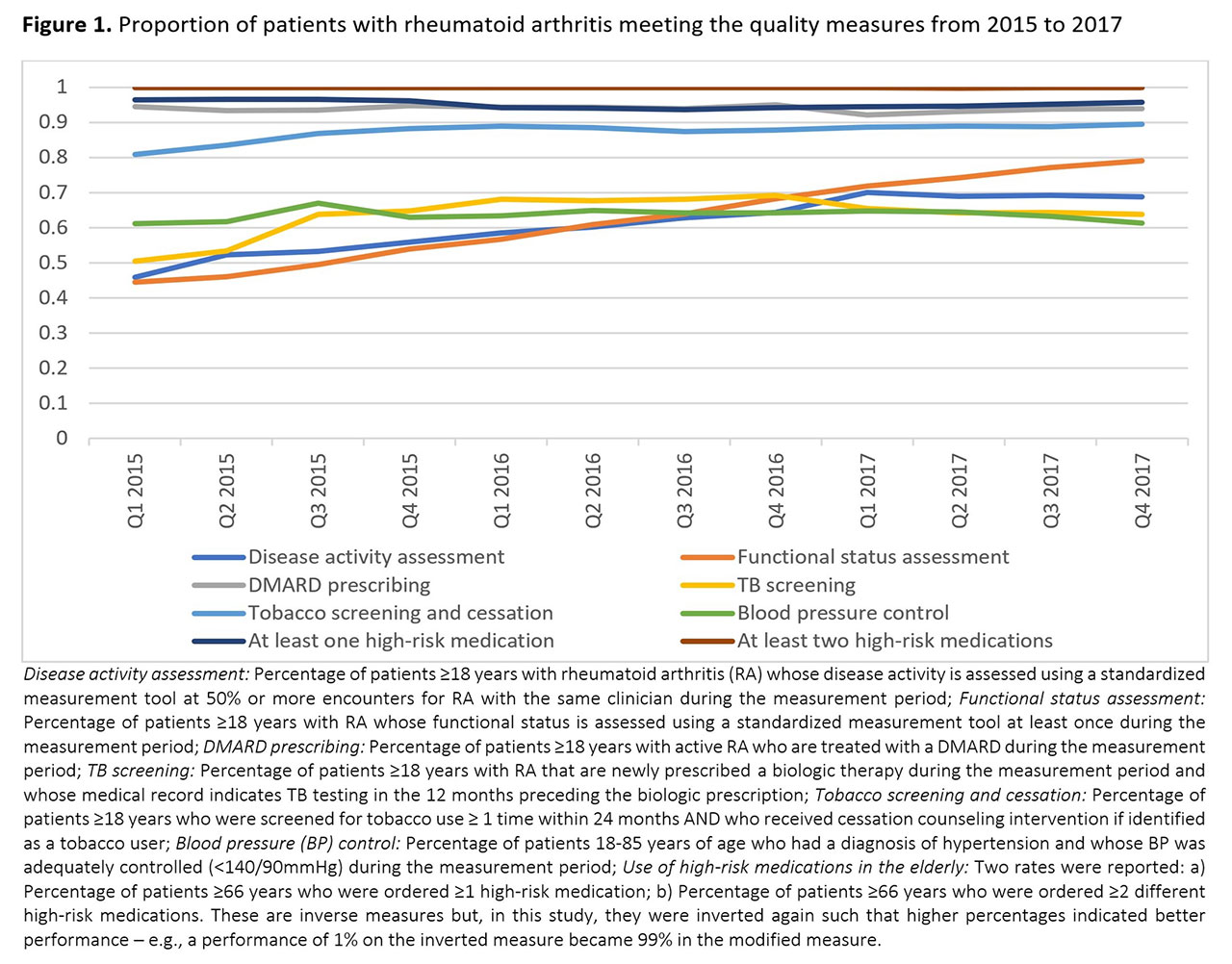
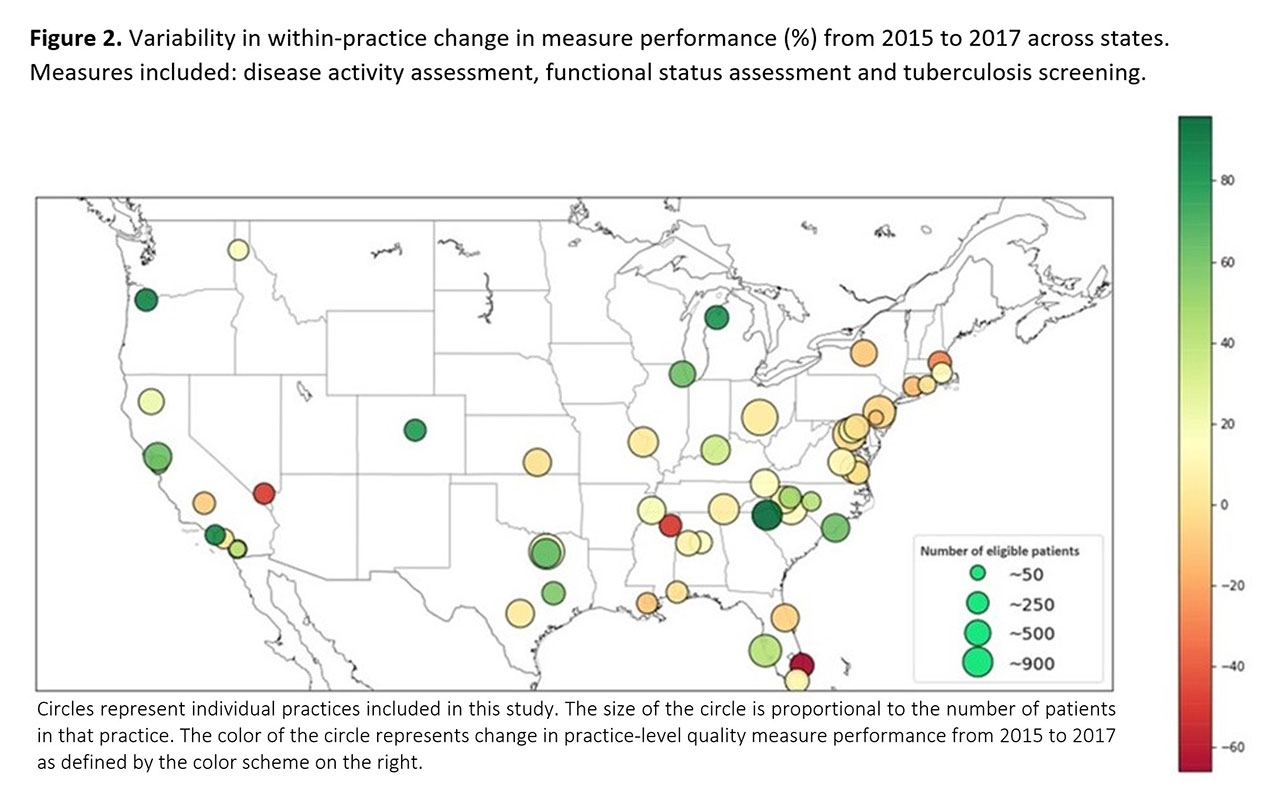
Results: Data from 59,986 patients from 54 practices was examined. Mean age was 62±14 years, 77% were female, 69% were Caucasian, and 81% had private insurance. The most common practice structure was a single-specialty group practice (46%), most practices had 1-4 providers (59.3%), and NextGen was the most commonly used EHR vendor (63%). From 2015 to 2017 there were clinically meaningful and statistically significant changes for disease activity assessment (8.4% per year, p< 0.001), functional status assessment (13.9% per year, p< 0.001), and TB screening (4.3% per year, p< 0.001), but only very modest changes for DMARD prescribing (1.0% per year, p=0.004), tobacco screening and cessation (2.9% per year, p< 0.001), and BP control (1.6% per year, p=0.022) (Figure 1). The degree of change in performance varied considerably across practices and regions (Figure 2). In adjusted analyses, single specialty group practices had the highest rates of improvement on disease activity assessment (12.8% per year), functional status assessment (17.3%) and TB screening (5.7%), while health systems were worsening over time on these measures (-18.5%, -4.2%, -19.3%, respectively; p-value for interaction ≤0.008).
Conclusion: Among practices participating in RISE from 2015 to 2017, aggregated performance, especially on RA-specific measures improved, although we found significant variation in performance over time between practices. These findings suggest that future work to identify workflow patterns leading to high performance or to dramatic improvements in quality are warranted.
Disclaimer: This data was supported by the ACR’s RISE Registry. However, the views expressed represent those of the authors, not necessarily those of the ACR.
To cite this abstract in AMA style:
Izadi Z, Schmajuk G, Kay J, Evans M, Yazdany J. The ACR’s Rheumatology Informatics System for Effectiveness (RISE) Demonstrates Improvements in Many Measures of Quality of Care Between 2015 and 2017 [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-acrs-rheumatology-informatics-system-for-effectiveness-rise-demonstrates-improvements-in-many-measures-of-quality-of-care-between-2015-and-2017/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-acrs-rheumatology-informatics-system-for-effectiveness-rise-demonstrates-improvements-in-many-measures-of-quality-of-care-between-2015-and-2017/