Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Cardiovascular morbidity and mortality are increased in axial spondyloarthritis (axSpA). The 2013 American College of Cardiology/American Heart Association (ACC/AHA) guidelines recommend high intensity statin therapy for primary prevention for 10-year atherosclerotic cardiovascular disease (ASCVD) risk scores ≥ 7.5%. We conducted a cross-sectional study evaluating the ASCVD risk profile of patients with axSpA compared to the general US population.
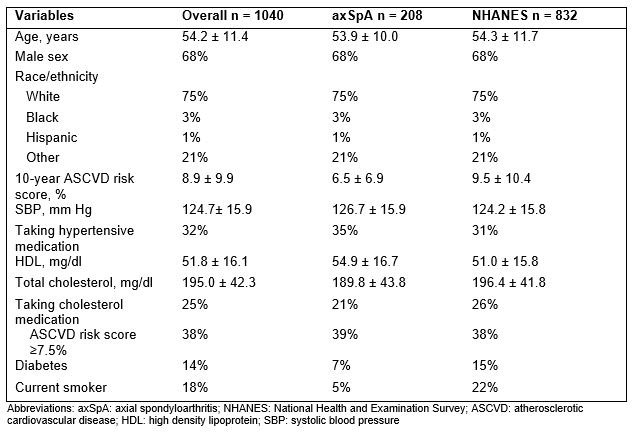
Methods: We included adults 18 years and older with AS by the modified New York criteria or non-radiographic axSpA by the ASAS criteria, who were followed longitudinally at two sites. After exclusion of ages outside the range of 40-75 years and patients without available cholesterol measures or blood pressures, 208 axSpA patients were included in the analysis. Other variables of interest were singly imputed using the last observation carried forward to the time of the cholesterol measurements. For general population comparators, we used individuals from the 2009-2014 National Health and Examination Survey (NHANES) cycles, who had available data for ASCVD risk score calculation by the Pooled Cohort Equation. Comparators from NHANES were matched 4:1 to subjects with axSpA on age, sex, and race. We performed descriptive statistics and estimated the prevalence ratio for a 10-year ASCVD risk score ≥7.5% comparing AS and matched NHANES comparators using conditional Poisson regression. We performed the same analysis among the subset of patients with AS (n=158).
Results: Overall, subjects had a mean ± SD age of 54.2 ± 11.4years, 68% were male, and 75% were white. The mean 10-year ASCVD risk score was 6.5 ± 6.9% for those with axSpA and 9.5 ± 10.4% for NHANES comparators. Compared to those with axSpA, the prevalence of current smoking and diabetes was higher among NHANES comparators. The estimated prevalence ratio for a 10-year ASCVD risk score ≥7.5% comparing those with axSpA and their age-, sex-, and race-matched comparators was 0.94 (95% CI, 0.83-1.05). Similar results were seen among the subset of patients with AS.
Conclusion: In our study, the prevalence of a 10-year ASCVD risk score ≥7.5% was not significantly different comparing patients with axSpA and those drawn from the general population, who were similar in terms of age, sex, and race. The increased CV risk associated with axSpA may be underestimated by this risk score calculation. Although axSpA patients may be at lower CV risk overall due to heterogenous disease severity, similar results were seen among an AS subset. In addition, further interpretation of these findings is limited by the small sample size and lack of information on socioeconomic status. Additional investigation of the performance of ASCVD risk scores in patients with axSpA is needed.
To cite this abstract in AMA style:
Liew J, Reveille J, Sawhney H, Castillo M, Naovarat B, Heckbert S, Gensler L. Ten-year Atherosclerotic Cardiovascular Disease Risk Scores in Axial Spondyloarthritis versus the General Population: A Cross-sectional Study [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/ten-year-atherosclerotic-cardiovascular-disease-risk-scores-in-axial-spondyloarthritis-versus-the-general-population-a-cross-sectional-study/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/ten-year-atherosclerotic-cardiovascular-disease-risk-scores-in-axial-spondyloarthritis-versus-the-general-population-a-cross-sectional-study/