Session Information
Date: Tuesday, November 9, 2021
Title: Vasculitis – Non-ANCA-Associated & Related Disorders Poster II (1862–1888)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Takayasu’s arteritis (TAK) is an idiopathic inflammatory disease primarily affecting the aorta and its major branches. Mycobacterium tuberculosis is prevalent in developing countries and can cause latent or active tuberculosis (TB) of the lung or other organs. Increased prevalence of TB has been reported in TAK but a causal relationship has not been established. The study objective was to determine if clinical characteristics differ among patients with TAK with known TB exposure.
Methods: Patients with TAK were recruited to a prospective observational cohort. All patients fulfilled the 1990 ACR Classification Criteria for TAK. TB was identified by medical history and/or Quantiferon-Gold screening. Categorical and continuous variables were compared using the Fisher’s exact test and Mann-Whitney test, respectively. Vascular calcification was based on radiology report of high-density lesions consistent with calcium deposition in large- or medium-size arterial territories on CT scans. Relapse was defined as clinical assessment showing recurrence of active vasculitis requiring escalation of immunosuppressive therapy after a period of stable remission. Incidentally found was defined as receiving diagnostic work up for non-TAK non-TB related indications which leads to unexpected discovery of vascular pathology. Asymptomatic was defined as complete absence of any vascular or systemic symptoms.
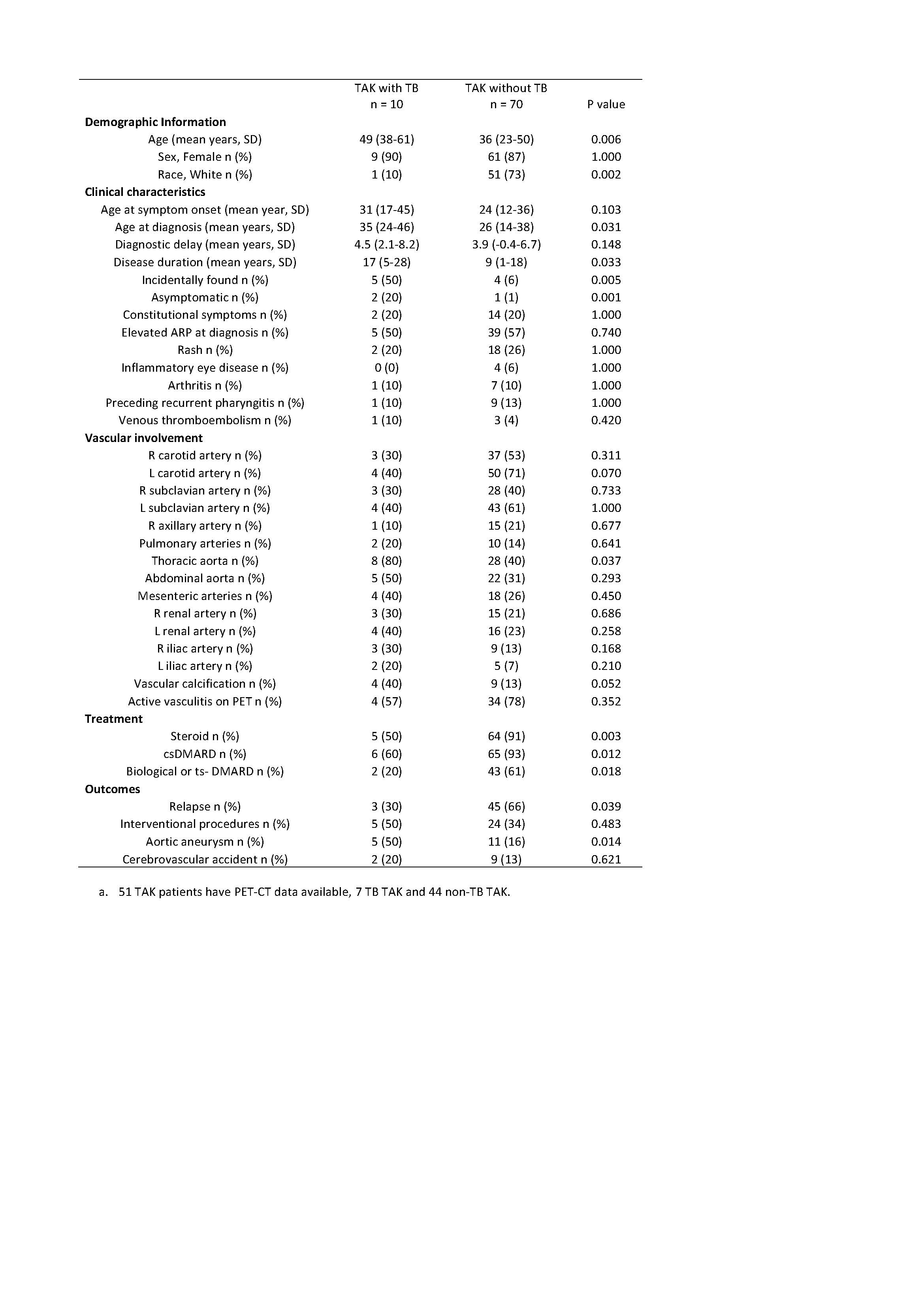
Results: Among 80 patients with TAK, 10 patients had a history of TB. 8 patients had latent TB, 1 patient had TB endometritis, and 1 patient had TB lymphadenitis and erythema induratum. All patients with active TB completed anti-active TB treatment. 7 of out 8 patients with latent TB completed anti-latent treatment and 1 patent with latent TB was recommended to start treatment. The majority of the patients were female (9 (90%) in TB-TAK and 61 (87%) in non-TB TAK). Compared to those without TB, TAK patients with TB were older at diagnosis (35 vs 26 years, p = 0.03) and less likely to be Caucasian (9 (10%) vs 51 (73%), p = 0.002). TAK patients with TB had longer disease duration (17 vs 9 years, p = 0.03), were more likely to be asymptomatic at diagnosis (2 (20%) vs 1 (1%), p = 0.001) or diagnosed based on incidentally found vascular pathology (50% vs 6%, p = 0.005). Patients with TB-TAK had distinct patterns of vascular disease, including increased thoracic aorta involvement (80% vs 40%, p = 0.037), aortic aneurysms (5 (50%) vs 4 (16%), p = 0.01), and vascular calcification (4 (40%) vs 9 (13%), p = 0.05). In terms of treatment, patients with TAK-TB were less likely to have ever received treatment with glucocorticoids (5 (50%) vs 64 (91%), p = 0.003), DMARDs (6 (60%) vs 65 (93%), p = 0.012), or biologics (2 (20%) vs 43 (61%), p = 0.018). Despite receiving less treatment, relapse was less frequent in patients with TB-TAK (3 (30%) vs 45 (66%), p = 0.039).
Conclusion: Patient with TAK and TB have unique clinical characteristics. Compared to other patients, patients with TAK and TB are more likely to have clinically indolent disease, have more structural damage to the aorta, receive less treatment, and are less likely to experience relapse. These data provide preliminary evidence in support of a potential causal relationship between TAK and TB.
To cite this abstract in AMA style:
Luo Y, Quinn K, Ferrada M, Novakovich E, Grayson P. Takayasu Arteritis Patients with Tuberculosis Have Unique Clinical Characteristics [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/takayasu-arteritis-patients-with-tuberculosis-have-unique-clinical-characteristics/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/takayasu-arteritis-patients-with-tuberculosis-have-unique-clinical-characteristics/