Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with Rheumatic Immune Diseases (RD) are at high risk for developing active tuberculosis (ATB). Accurate and timely diagnosis of ATB in RD patients is crucial. Interferon-gamma release assays (IGRAs) and the tuberculin skin test (TST) are immunological diagnostic methods recommended by expert consensus in China for the auxiliary diagnosis of ATB. However, the accuracy of these methods in RD patients has not been well-studied. This study aims to compare the diagnostic accuracy of TST and T-SPOT.TB in RD patients presenting with suspected tuberculosis symptoms.
Methods: Between September 2014 and September 2015, RD patients presenting with any of suspected tuberculosis symptoms (fever, cough, night sweats, unexplained weight loss) were prospectively enrolled. Patients underwent both T-SPOT.TB and TST tests. Based on clinical routine diagnostics, patients were classified into ATB (including bacteriologically confirmed and clinically diagnosed cases) and non-ATB groups. ROC curves were drawn to compare the accuracy of T-SPOT.TB and TST in diagnosing ATB and to determine the optimal cut-off values. Sensitivity, specificity, predictive values, and likelihood ratios were calculated to evaluate the diagnostic consistency of T-SPOT.TB and TST.
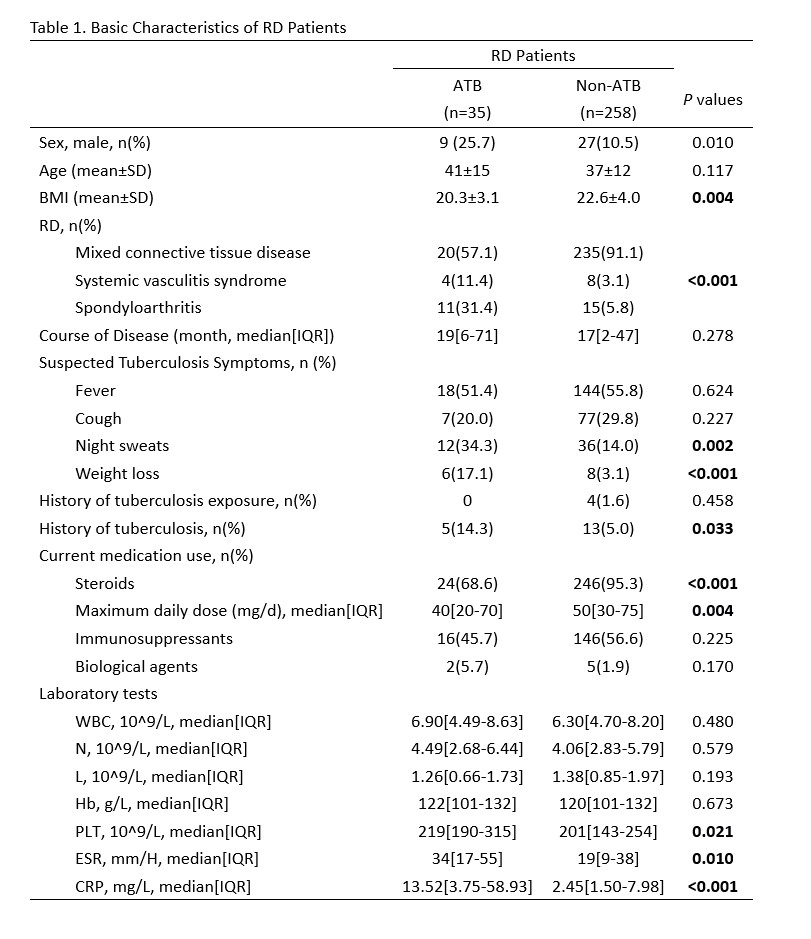
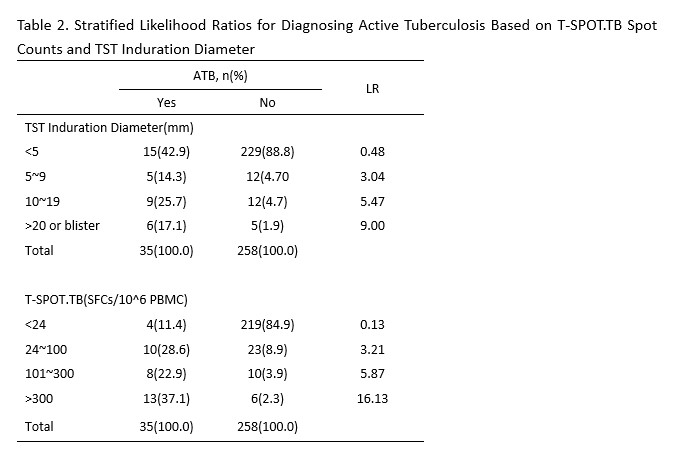
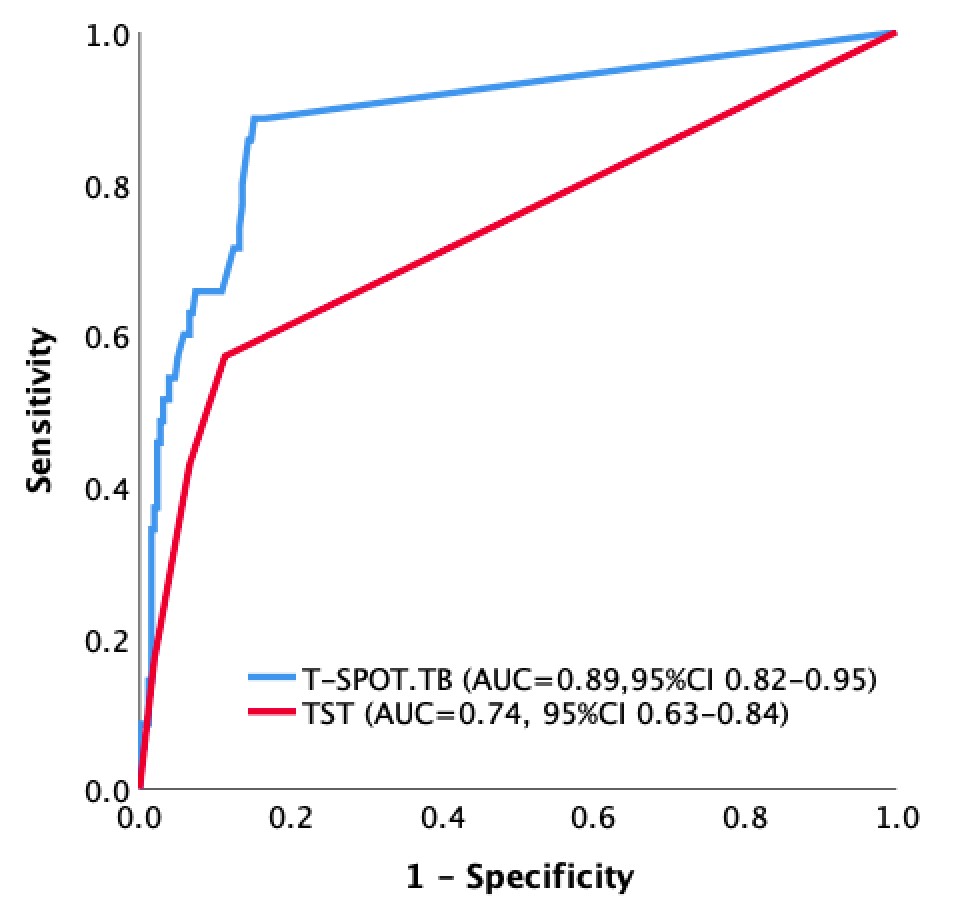
Results: A total of 300 RD patients were enrolled, with 35 (11.7%) diagnosed with ATB and 258 (86.0%) excluding ATB. The diagnosis was unclear in 7 cases (2.3%). RD patients with ATB had significantly higher rates of night sweats (34.3% vs. 14.0%, p=0.003) and unexplained weight loss (17.1% vs. 3.1%, p< 0.001) compared to the non-ATB group, while fever and cough showed no significant differences between the groups. The AUROC for T-SPOT.TB in diagnosing ATB was 0.89 (95%CI 0.82-0.95), significantly higher than the AUROC for TST at 0.74 (95%CI 0.63-0.84) (difference in AUROC 0.15, 95% CI 0.06-0.24, p=0.001). The optimal cut-off for T-SPOT.TB was 24 SFCs/10^6 PBMC, with sensitivity, specificity, positive likelihood ratio, negative likelihood ratio, positive predictive value, and negative predictive value of 88.6%(95%CI 73.3%-96.8%), 84.9%(95%CI 79.9%-89.0%), 5.86(95%CI 4.29-8.01), 0.13(95%CI 0.05-0.34), 44.3%(95%CI 32.4%-56.7%), and 98.2%(95%CI 95.5%-99.5%), respectively. For TST, the optimal cut-off was an induration diameter of 5mm, with respective values of 57.1%(95%CI 39.4%-73.7%), 88.8%(95%CI 84.3%-92.3%), 5.08(95%CI 3.25-7.95), 0.48(95%CI 0.33-0.71), 40.8%(95%CI 27.0%-55.8%), and 93.9%(95%CI 90.1%-96.5%). The sensitivity of T-SPOT.TB was significantly higher than that of TST (p=0.003), while specificity did not differ significantly (p=0.193). The likelihood ratio for diagnosing ATB increased with higher T-SPOT.TB spot counts and larger TST indurations. The agreement between T-SPOT.TB and TST in diagnosing ATB was moderate (kappa=0.466, p< 0.001), and parallel testing did not enhance the sensitivity of T-SPOT.TB.
Conclusion: Both T-SPOT.TB and TST have auxiliary diagnostic value for ATB in RD patients presenting with suspected symptoms. T-SPOT.TB is more accurate than TST, particularly in terms of sensitivity. Higher T-SPOT.TB spot counts or larger TST indurations should raise suspicion of possible ATB co-infection.
To cite this abstract in AMA style:
Zhang L, Li Y, Wang H, Liu X. T-SPOT.TB and TST in Diagnosing Active Tuberculosis in Patients with Rheumatic Immune Diseases: A Fully Paired Comparative Diagnostic Test Accuracy Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/t-spot-tb-and-tst-in-diagnosing-active-tuberculosis-in-patients-with-rheumatic-immune-diseases-a-fully-paired-comparative-diagnostic-test-accuracy-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/t-spot-tb-and-tst-in-diagnosing-active-tuberculosis-in-patients-with-rheumatic-immune-diseases-a-fully-paired-comparative-diagnostic-test-accuracy-study/