Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Prior research suggests that systemic inflammation contributes to the pathogenesis of depression, but longitudinal studies in patients with rheumatoid arthritis (RA) are lacking. Comorbid depression is common in patients with RA and traditional risk factors such as disability, fatigue, and pain explain only a portion of the increased prevalence of depression in RA. We prospectively examined the association between serum C-reactive protein (CRP) and depression to determine whether an increase in CRP precedes an increase in depressive symptoms in adults with RA.
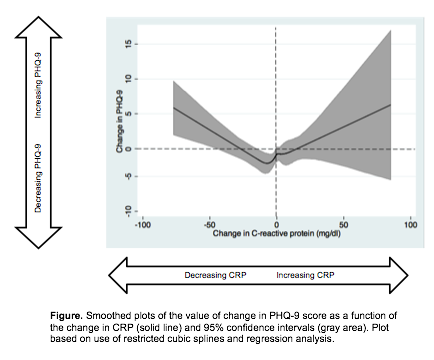
Methods: Participants were patients from a multi-site observational RA cohort. Inclusion criteria for this analysis included age ≥ 18 years of age, meeting the American College of Rheumatology classification criteria for RA, and at least two clinical visits that included a measure of depression, the Patient Health Questionnaire-9 (PHQ-9), and two measurements of serum high-sensitivity CRP. In order to calculate a change in CRP that occurred prior to the change in depression score, the first CRP was collected up to 6 weeks prior to the first PHQ-9 score, and the second CRP was collected up to 6 weeks prior to the second PHQ-9 score. Given the non-linear relationship between predictor and outcome, odds ratios were estimated using a restricted cubic spline regression analysis. Post-estimation Wald test confirmed there was a non-linear relationship between changes in CRP and successive PHQ-9 scores.
Results: There were 362 observations for 212 patients with a pair of clinical visits with two serum CRP measurements and a subsequent change in PHQ-9 score measured. The mean ± SD of the 1st CRP and change in CRP were 8.6 ±13 and 0.14 ±12, respectively. With regard to the prevalence of depressive symptoms, 41% of patients scored > 10 on the PHQ-9 during at least one clinic visit, which corresponds to a symptom severity of at least moderate depression. The mean ± SD of the 1st PHQ-9 and change in PHQ-9 was 6 ±5 and -0.2 ±4, respectively corresponding to an initial symptom severity of mild depression. A significant non-linear relationship existed (p<.001) between change in CRP and change in depression score in patients with RA (Figure). Adjustment for age, gender, race/ethnicity, body mass index, and socioeconomic status did not significantly alter results.
Conclusion: An increase in systemic inflammation as measured by CRP contributes to an increase in depressive symptoms in a subset of patients with RA. For these patients, further investigation is warranted as to whether treating RA with additional anti-inflammatories may have the extra benefit of decreasing depression.
Disclosure:
M. Margaretten,
None;
L. Trupin,
None;
P. P. Katz,
None;
G. Schmajuk,
None;
J. Yazdany,
None;
C. Tonner,
None;
J. Barton,
Pfizer,
2;
E. H. Yelin,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/systemic-inflammation-contributes-to-depression-in-patients-with-rheumatoid-arthritis/