Session Information
Session Type: ACR Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Pulmonary involvement, including pulmonary vascular disease and interstitial lung disease can be an important cause of morbidity and even mortality in patients with primary systemic vasculitides (PSV). Outcomes of lung transplantation (LTx), a potentially life-saving intervention for patients with advanced pulmonary disease in patients with underlying autoimmune conditions including systemic sclerosis (SSc) and connective tissue disease-related ILD (CTD-ILD) are comparable to those of patients without underlying autoimmune conditions. Outcomes of LTx in patients with PSV have not been reported other than descriptively in scattered case reports. The aim of this study is to describe survival after transplantation in patients with PSV undergoing LTx and compare that to survival in LTx patients with SSc and non-CTD-ILD.
Methods: We conducted a retrospective cohort study of adult who underwent LTx in the United States between January 1996 and May 2018. Data was provided by UNOS, a non-profit organization that records data on all solid organ transplants performed in the US. Subjects from the thoracic transplant databases were included if they were at least 18 years of age and had diagnostic codes for PSV. Diagnosis of PSV included: Takayasu’s arteritis (TAK), Granulomatosis with Polyangiitis (GPA), Eosinophilic Granulomatosis with Polyangiitis (EGPA) and Microscopic Polyangiitis (MPA). Age (within a 5-year range) and sex-matched controls undergoing LTx were identified for 2 other groups of transplanted patients: 1) Patients with a primary diagnosis of SSc and 2) Patients with a diagnosis of ILD (not CTD-ILD) and selected in a 1:1:1 ratio. We compared patient survival using Kaplan-Meier estimates and a Kruskal-Wallis test.
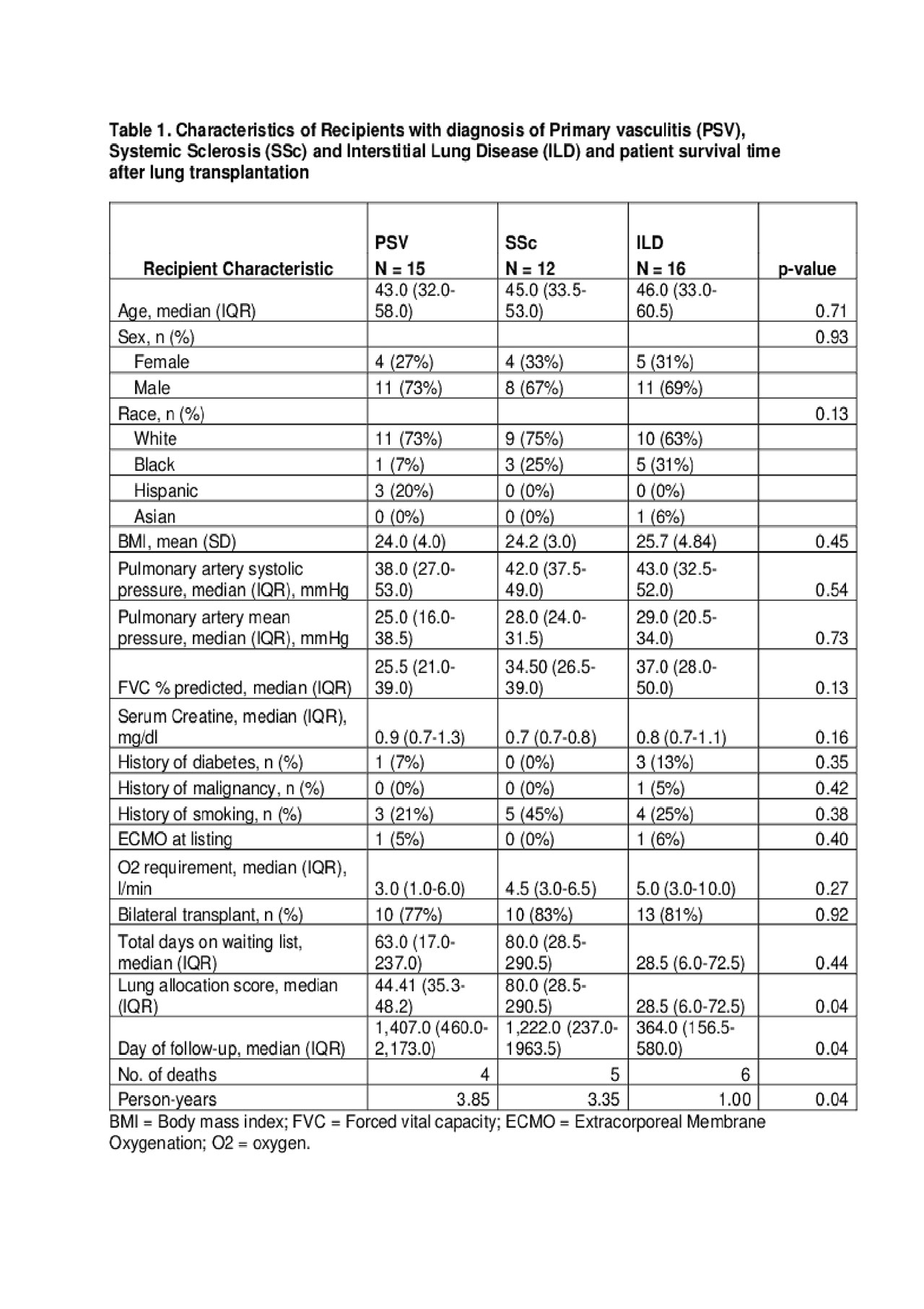
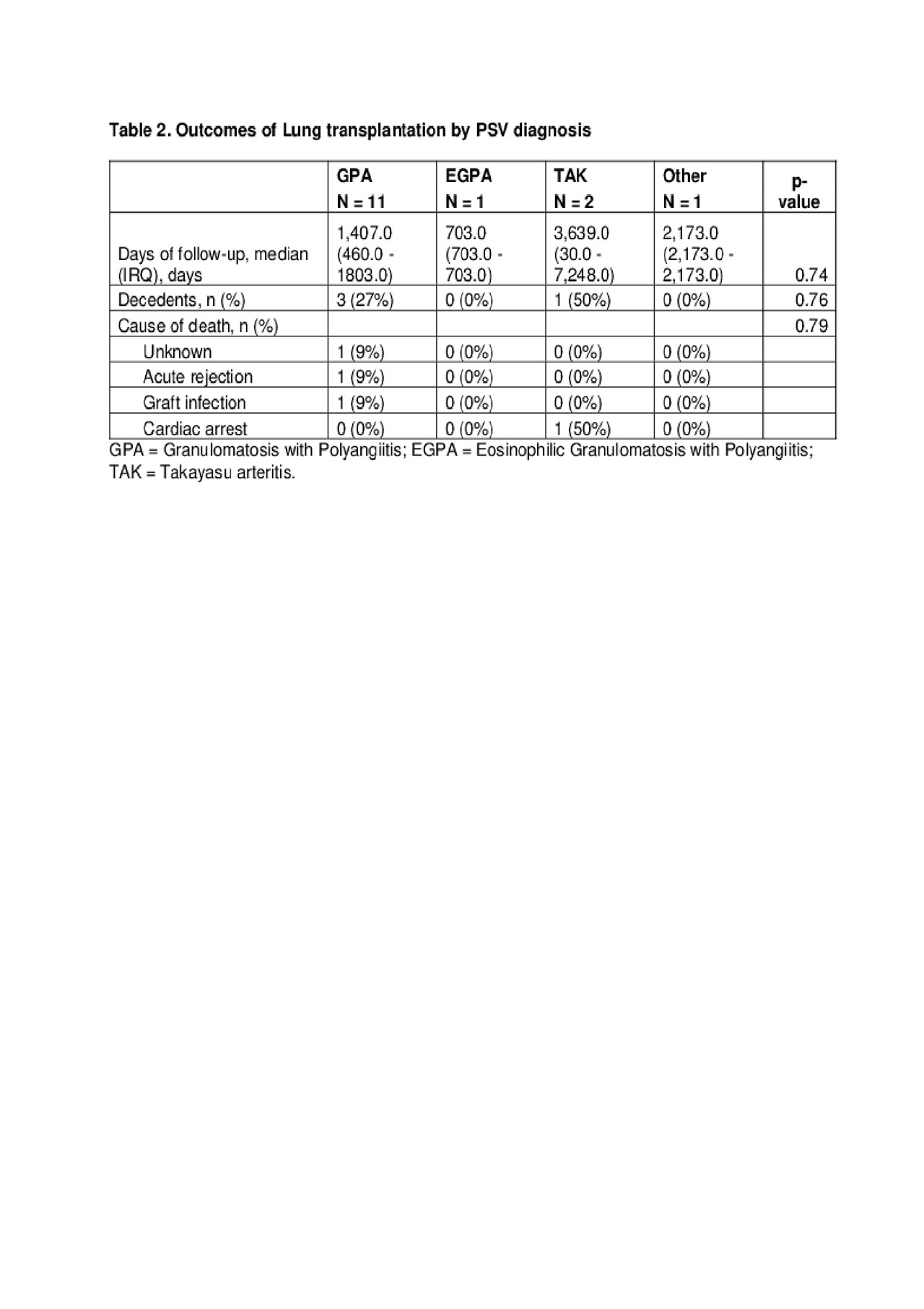
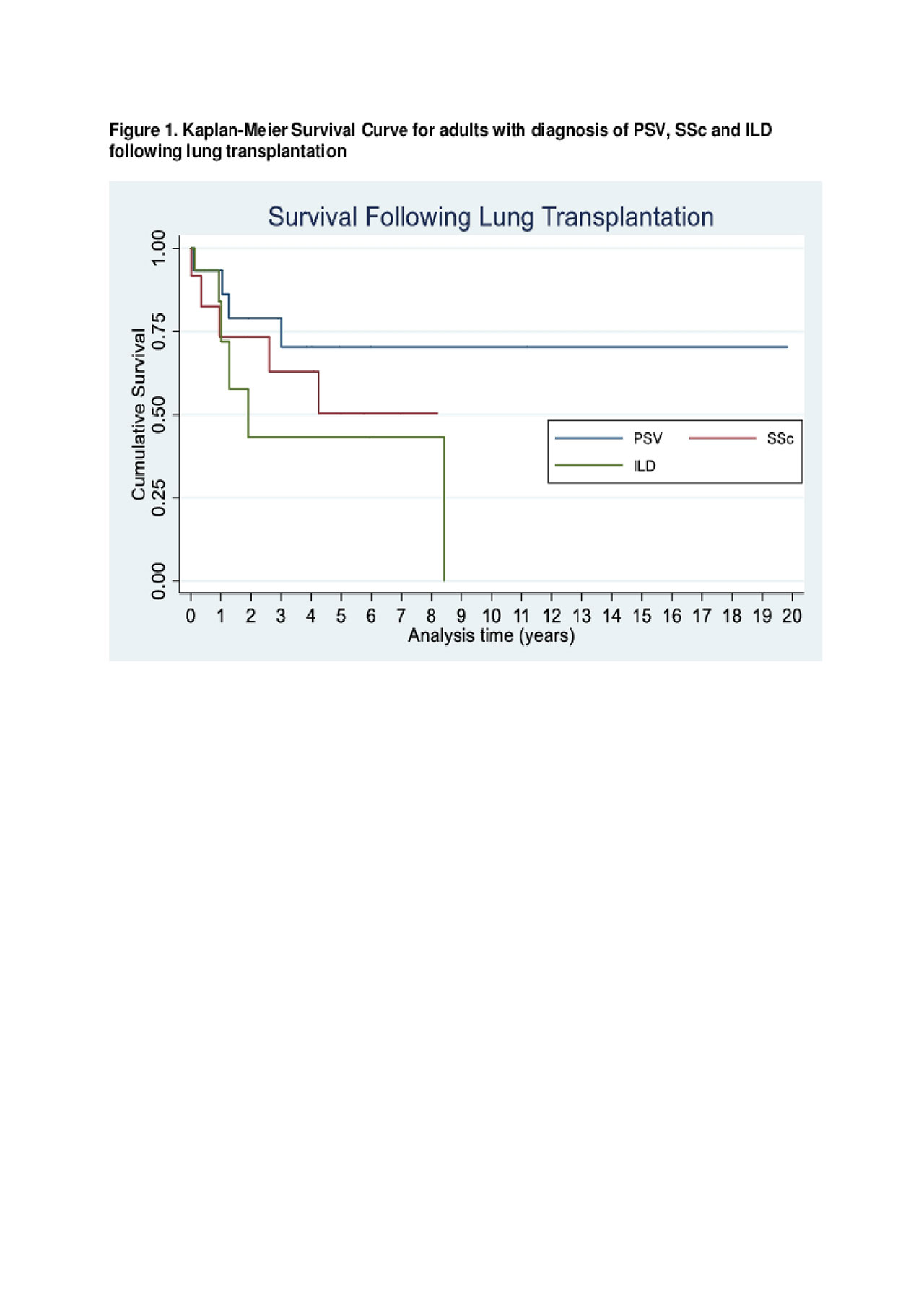
Results: 23 patients with PSV were identified in the thoracic transplant database. Of these, 2 patients underwent heart transplant (1 EGPA, 1 TAK) and 1 patient with diagnosis of GPA had a lung and heart transplant. 20 patients with a diagnosis of PSV were listed only for LTx, of those only 15 underwent LTx. 73% were male, with a median age 43 years and 73% were white (Table 1). GPA was the most common diagnosis (73%) (Table 2). Except for 1 patient with a diagnosis of TAK, all patients underwent LTx after May 4, 2005 (implementation of Lung Allocation Score). Patients with a diagnosis of PSV and SSc had a longer duration on waiting list compared to ILD patients (p = 0.04). Otherwise, there were no significant differences among baseline recipient characteristics between groups. Patients with PSV and SSc had a longer survival time compared to ILD (p = .040) (Figure 1). There were no differences in survival or cause of death between PSV diagnoses.
Conclusion: To our knowledge, this is the first analysis reporting outcomes of patients with PSV undergoing LTx. PSV remains a rare context for LTx. There were no significant differences in patient survival time between PSV and SSc. Although this study has limitations, in particular small sample size, our data suggest that lung transplantation in patients with PSV achieved comparable outcomes to those in patients with SSc and better than ILD patients and should be considered a therapeutic option in this patient population.
To cite this abstract in AMA style:
Sattui S, Abutalib Z, Finik J, Spiera R. Survival After Lung Transplantation in Adults with Primary Systemic Vasculitides: Analysis of the United Network of Organ Sharing (UNOS) Database [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/survival-after-lung-transplantation-in-adults-with-primary-systemic-vasculitides-analysis-of-the-united-network-of-organ-sharing-unos-database/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/survival-after-lung-transplantation-in-adults-with-primary-systemic-vasculitides-analysis-of-the-united-network-of-organ-sharing-unos-database/