Session Information
Session Type: Patient Perspectives Poster Session
Session Time: 12:00PM-2:00PM
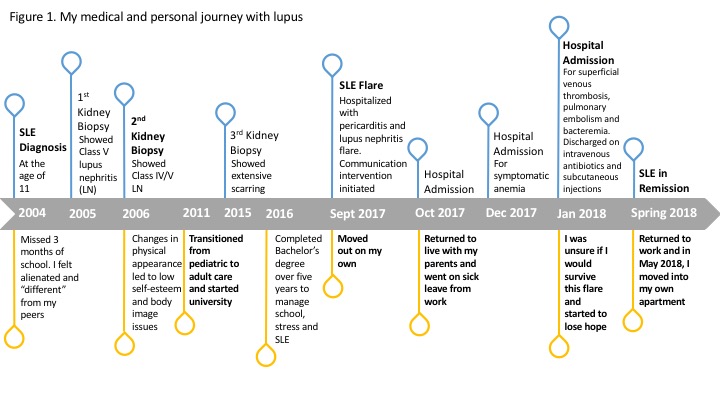
Background/Diagnosis: I was diagnosed with systemic lupus erythematosus (SLE) at the age of eleven and have experienced multiple SLE flares, hospitalizations, invasive procedures and complex treatment plans. My journey with SLE has at times made me feel isolated, affected my body image and self-esteem. While living with these challenges, I completed a Bachelor’s degree and began a career. In 2017, a severe SLE flare left me on sick leave and often unable to perform basic daily tasks due to pain, fatigue and weakness, forcing me to return to live with my parents. My journey with lupus is outlined in Figure 1.
Treatment: Cecilia’s care team recognized the challenges she faced managing her latest SLE flare. As an interprofessional team, a care plan was developed and strategies implemented to promote patient-centered communication and improve disease management. As part of the care plan, regular communications with Cecilia were prompted by her healthcare team after each admission and change in treatment. Communication was predominantly nurse-led, via email, and covered symptoms, medications and side effects, and coping. Open-ended questions engaged Cecilia in identifying and prioritizing symptoms or concerns. Frequency of contact varied according to severity of symptoms or complexity of treatments, and often was weekly. Regular contact provided opportunities to improve symptom management, assistance and encouragement in managing treatments, and facilitated timely access to her rheumatology/nephrology team.
Maintenance: The interventions improved my self-management of SLE, engagement with my healthcare team and my resiliency during a stressful period of my life. Transitioning from pediatric to adult care, I felt I was a patient file, an “interesting case.” By recognizing and responding to the challenges I was facing, I felt my healthcare team was invested in my care and thought of me as a person. Prompting me to check-in with myself increased my capacity to alert my team to symptoms or complications, seek urgent medical attention when needed, and manage intravenous antibiotics and subcutaneous injections at home. Increased self-awareness, paired with a receptive team, encouraged my involvement in clinic appointments and treatment decisions, and to seek additional supports, such as online support groups. My symptoms have significantly improved, I am tapering my prednisone dose and have returned to work. This resiliency helped me persevere and led me to where I am today—healthier and happier than I was before this flare began.
Quality of Life: My quality of life has greatly improved since the intervention and recovery from my SLE flare. I am able to perform basic daily tasks again, live on my own, and participate in activities I love, such as exercising. I am more confident about the future knowing I have the support of my healthcare team and the resiliency to live well with lupus.
To cite this abstract in AMA style:
Amoakohene C, Sanchez-Guerrero J, Urowitz M, Gladman DD, Touma Z, Wakani L. Strengthening My Resiliency: How My Interprofessional Healthcare Team and I Improved My Management of Lupus [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/strengthening-my-resiliency-how-my-interprofessional-healthcare-team-and-i-improved-my-management-of-lupus/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/strengthening-my-resiliency-how-my-interprofessional-healthcare-team-and-i-improved-my-management-of-lupus/