Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose:
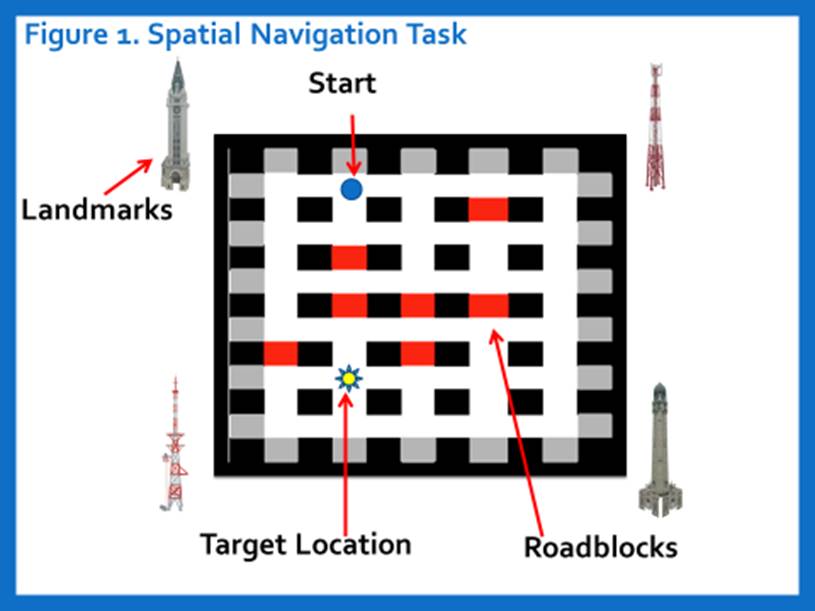
Cognitive impairment is well-documented in SLE with considerable impact on quality of life but attribution is limited by a lack of biomarkers that distinguish SLE disease-related mechanisms from other causes (medications, infection, mood disorders, thrombosis). Cross-reactive anti-dsDNA/NMDA receptor antibodies (DNRAb) have been shown to bind neurons in the mouse hippocampus, specifically place cells, with resulting synaptic signaling changes promoting neuron dysfunction or death and difficulties in spatial tasks1. The purpose of this study was to evaluate serum DNRAb associations with spatial memory in SLE using a novel spatial navigation task (SNT).
Methods:
21 SLE patients that met ACR criteria, had no history of CNS insult and low disease activity and 9 age, gender and ethnically matched healthy controls (HC) were recruited. SLE disease activity was assessed by SLEDAI within 2 weeks of testing. The SNT utilizes a desktop virtual environment to assess spatial memory. Participants were placed at a start point and asked to navigate through a computerized virtual city of 30 intersections (Fig. 1), with one unmarked target intersection set to trigger a congratulatory screen upon entry. Subjects were given a maximum of 5 minutes to complete each of 4 trials to find the target. Serum DNRAb assays were performed by ELISA with the DWEYS consensus sequence. Analyses included the Chi Square and student t tests.
Results:
Table 1 shows relevant subject characteristics with SLE subjects grouped by DNRAb titer. DNRAB- SLE subjects had slightly higher SLEDAI scores and frequency of anti-DNA antibody titers compared to the DNRAb+ group. Over 4 trials, 77.7% of HC found the target compared to 20% of DNRAb+ subjects (p=.01). DNRAb- SLE behaved like HC with a 60% success rate (p=.41). Differences between DNRAb+ and – did not reach statistical significance (p=.07). These differences in success occurred despite all three groups making the same number of movements (p=.83) and turns (p=.49) during the trials, covering the same amount of search area (p=.76), having a similar amount of computer experience (p=.15), and no differences in simple reaction time tasks (p=.7).
Conclusion:
DNRAb+ subjects perform poorly on the SNT compared to DNRAb- SLE subjects who perform similarly to HC. The lack of group differences for mood disturbances, medications and demographics and that the DNRAb- group performed similar to HC despite having higher disease activity and anti-DNA titers suggest that this SNT may provide an objective measure of DNRAb-mediated brain toxicity that will need to be replicated in future studies.
1Chang, EH.EBioMedicine. 2015;2(7)
|
Table 1. Subject Characteristics |
||||||
|
SLE n=21 |
Healthy control n=9 |
p SLE vs HC |
SLE DNRAb+ n=10 |
SLE DNRAb- n=11 |
p SLE+ vs SLE- |
|
|
Age |
42.3 ± 10.5 |
38.6 ± 11.7 |
.455 |
45.6 ± 9.5 |
38.1 ± 10.4 |
.099 |
|
Gender: male |
2 (9.5%) |
0 |
.338 |
0 |
2 (18%) |
.156 |
|
Ethnicity |
|
|
.59 |
|
|
.313 |
|
Latino/ Hispanic |
4 (20%) |
3 (37.5%) |
|
3 (30%) |
1 (9%) |
|
|
Asian |
1 (5%) |
1 (12.5%) |
|
0 |
1 (9%) |
|
|
African American |
14 (70%) |
4 (50%) |
|
6 (60%) |
9 (82%) |
|
|
Caucasian |
1 (5%%) |
0% |
|
1 (10%) |
0 |
|
|
Education |
13.4 ± 2.4 |
15.3 ± 2.4 |
.08 |
13.1 ± 2.3 |
13.4 ±2.5 |
.808 |
|
Computer experience; some/none |
10 (48%) |
1 (11%) |
.057 |
7 (70%) |
3 (27%) |
.05* |
|
Disease duration |
|
|
|
16 ± 9.1 |
11.1 ± 8.9 |
.227 |
|
SLEDAI |
|
|
|
1.1 ± 1.4 |
3.1 ± 2.3 |
.026* |
|
SLICC DI |
|
|
|
.9 ± 1.0 |
.91 ± 1.2 |
.985 |
|
Beck Depression Index |
7.1 ± 5.4 |
1.8 ± 2.4 |
.001 |
5.5 ± 5 |
8.6 ± 5.5 |
.204 |
|
STA-Y (anxiety) |
30.7 ± 9.2 |
25.1 ± 5.2 |
.1 |
32.3 ± 10.1 |
29.2 ± 8.4 |
.45 |
|
Medications |
|
|
|
|
|
|
|
Current .1 (mg/day) |
|
|
|
1.8 ± 2.9 |
3.2 ± 4.2 |
.379 |
|
Current HCQ |
|
|
|
100% |
8 (73%) |
.074 |
|
Current DMARDa |
|
|
|
5 (50%) |
6 (55%) |
.835 |
|
anti-dsDNA ab + |
|
|
|
2 (20%) |
8 (73%) |
.016* |
|
anti-Ro+ |
|
|
|
8 (80%) |
8 (73%) |
.696 |
|
anti-La+ |
|
|
|
2 (20%) |
3 (27%) |
.696 |
|
anti-ribosomal P+ |
|
|
|
1 (10%) |
3 (27%) |
.314 |
|
Anticardiolipin/LAC+ |
0 |
|
|
0 |
0 |
|
To cite this abstract in AMA style:
Anderson E, Ploran EJ, Diamond B, Volpe B, Aranow C, Mackay M. Spatial Navigation Impairment Associated with Anti-NMDA Receptor Antibodies in Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/spatial-navigation-impairment-associated-with-anti-nmda-receptor-antibodies-in-systemic-lupus-erythematosus/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/spatial-navigation-impairment-associated-with-anti-nmda-receptor-antibodies-in-systemic-lupus-erythematosus/