Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Socioeconomic factors such as poverty may mediate racial disparities in health outcomes including those of total hip arthroplasty (THA), and confound analyses of differences between blacks and whites.
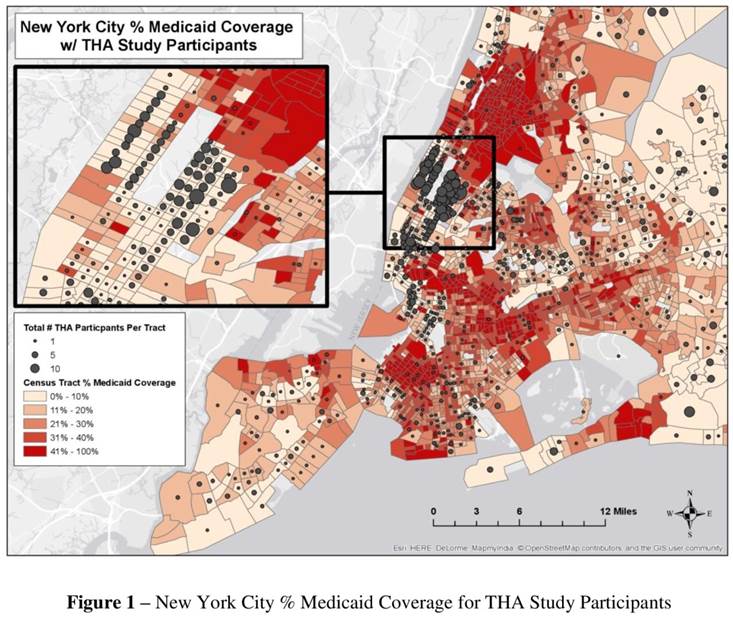
Methods: Using data from a large institutional THA registry, we compared pain and function 2 years after surgery between blacks and whites. The census tract variable “percent of the population with Medicaid insurance coverage” was used to measure community deprivation. We used geocoding to link patients to census tracts, built models that incorporated both individual patient and census tract data, and analyzed the interaction between race and percent of population with Medicaid coverage and its association with patient-reported outcomes 2 years after THA.
Results: Black patients, comprising 145/4170 (3%) of THA cases, had worse pain and function scores both at baseline and at 2 years after THA compared to whites (Table 1). There was a strong positive correlation between census tract Medicaid coverage and percent living below the poverty line (rho = 0.69; p<0.001). Racial disparities in 2-year WOMAC pain and function were magnified in communities with a high percentage of the population covered by Medicaid (Table 2). For blacks in these communities, 2-year WOMAC function scores were predicted to be 5.54 points lower (80.42 vs. 85.96) than in blacks from communities with a low prevalence of Medicaid coverage, while scores for whites did not differ between communities. Pain scores were also lower for blacks living in deprived areas, but the difference was not significant.
Conclusion: WOMAC pain and function 2 years after THA are similar among blacks and whites in communities with little deprivation (measured as percent of the population with Medicaid insurance coverage). WOMAC function at 2 years is worse among blacks in areas of higher deprivation, whereas this poverty gradient does not impact outcomes among whites.
|
Table 1: Characteristics of the cohort |
||||
|
Characteristic |
Total |
White |
Black |
P-Value |
|
Number of patients |
4170 (100%) |
4025 (97%) |
145 (3%) |
|
|
Age at surgery (years), mean (SD) |
65.29 (11.01) |
65.42 (10.98) |
61.69 (11.23) |
0.0002 |
|
Female, n (%) |
2311 (55.42%) |
2219 (55.13%) |
92 (63.45%) |
0.048 |
|
BMI (kg/m2), mean (SD) |
27.75 (5.48) |
27.68 (5.44) |
29.74 (6.33) |
0.0002 |
|
Hispanic, n (%) |
75 (1.80%) |
73 (1.81%) |
2 (1.38%) |
1.00 |
|
One or more comorbidities, n (%) |
1013 (24.29%) |
956 (23.75%) |
57 (39.31%) |
<0.0001 |
|
College or above, n (%) |
2805 (68.35%) |
2721 (68.69%) |
84 (58.74%) |
0.012 |
|
Insurance payer, n (%) Medicaid Medicare Other insurance |
53 (1.27%) 2317 (55.56%) 1800 (43.17%) |
30 (0.75%) 2257 (56.07%) 1738 (43.18%) |
23 (15.86%) 60 (41.38%) 62 (42.76%) |
<0.0001 |
|
ASA Class, n (%) Missing I-II III-IV |
2 3387 (81.26%) 781 (18.74%) |
2 3279 (81.51%) 744 (18.49%) |
0 108 (74.48%) 37 (25.52%) |
0.033 |
|
Hospital for Special Surgery Expectations Score, mean (SD) |
83.30 (16.46) |
83.17 (16.52) |
86.64 (14.42) |
0.043 |
|
WOMAC pain at baseline, mean (SD) |
53.58 (17.85) |
53.84 (17.72) |
46.48 (20.04) |
<0.0001 |
|
WOMAC pain at 2 Years, mean (SD) |
93.63 (11.39) |
93.81 (11.13) |
88.60 (16.39) |
<0.0001 |
|
Delta WOMAC pain, mean (SD)
|
40.04 (19.14) |
39.97 (18.95) |
42.15 (23.75) |
0.144 |
|
WOMAC function at baseline, mean (SD) |
49.93 (18.04) |
50.19 (18.00) |
42.78 (17.80) |
<0.0001 |
|
WOMAC function at 2 Years, mean (SD) |
90.86 (13.21) |
85.43 (16.09) |
77.80 (22.42) |
<0.0001 |
|
Delta WOMAC function, mean (SD) |
40.93 (19.31) |
40.89 (19.12) |
41.93 (24.22) |
0.351 |
|
Percent Below Poverty Level, n (%) <10% 10%-20% 20%-30% 30%-40% >40% |
3363 (80.69%) 626 (15.02%) 102 (2.45%) 51 (1.22%) 26 (0.62%) |
3303 (82.10%) 585 (14.54%) 82 (2.04%) 33 (0.82%) 20 (0.50%) |
60 (41.38%) 41 (28.28%) 20 (13.79%) 18 (12.41%) 6 (4.14%) |
<0.0001 |
|
Percent with Medicaid Coverage, n (%) <=10% 10%-20% 20%-30% 30%-40% >40% |
3128 (75.85%) 679 (16.46%) 194 (4.70%) 97 (2.35%) 26 (0.63%) |
3086 (76.71%) 644 (16.12%) 167 (4.18%) 77 (1.93%) 20 (0.50%) |
42 (32.31%) 35 (26.92%) 27 (20.77%) 20 (15.38%) 6 (4.62%) |
<0.0001 |
|
Table 2: WOMAC pain and function 2 years after total hip arthroplasty: interaction between race and percent of Medicaid coverage at census-tract level |
|||||||
|
Percent of Medicaid Coverage at Census-Tract Level |
Race |
WOMAC Pain at 2 Years* |
WOMAC Function at 2 Years** |
||||
|
Estimate (Standard Error) |
Est. Difference (Standard Error) |
P-Value |
Estimate (Standard Error) |
Est. Difference (Standard Error) |
P-Value |
||
|
10% |
Black White |
88.44 (1.59) 90.43 (1.05) |
-1.99 (1.29) |
0.12 |
85.96 (1.78) 87.95 (1.19) |
-1.99 (1.44) |
0.17 |
|
20% |
Black White |
87.54 (1.28) 90.13 (1.08) |
-2.59 (1.12) |
0.02 |
84.11 (1.43) 87.59 (1.22) |
-3.48 (1.26) |
0.01 |
|
30% |
Black White |
86.63 (1.38) 89.82 (1.16) |
-3.20 (1.45) |
0.03 |
82.27 (1.49) 87.23 (1.31) |
-4.96 (1.60) |
0.002 |
|
40% |
Black White |
85.72 (1.81) 89.52 (1.28) |
-3.80 (2.04) |
0.06 |
80.42 (1.93) 86.87 (1.45) |
-6.45 (2.24) |
0.004 |
|
50% |
Black White |
84.81 (2.41) 89.21 (1.44) |
-4.40 (2.74) |
0.11 |
78.57 (2.56) 86.51 (1.63) |
-7.94 (2.99) |
0.01 |
|
60% |
Black White |
83.91 (3.07) 88.91 (1.61) |
-5.01 (3.47) |
0.15 |
76.73 (3.28) 86.15 (1.83) |
-9.42 (3.78) |
0.01 |
|
*Estimation based on linear mixed-effect model assessing the effect of interaction between race and percent of Medicaid coverage at census-tract level on WOMAC pain at 2 years after THA, using the following assumptions: WOMAC pain at baseline=53; age at surgery=65; BMI=28/kg/m2; HSS expectation score=83; sex=female; comorbidities=0; insurance=Medicaid; education=college and above. ** Estimation based on linear mixed-effect model assessing the effect of interaction between race and percent of Medicaid coverage at census-tract level on WOMAC function at 2 years after THA, using the following assumptions: WOMAC function at baseline=49; age at surgery=65; BMI=28/kg/m2; HSS expectation score=83; sex=female; comorbidities=0; insurance=Medicaid; education=college and above. |
|||||||
 |
To cite this abstract in AMA style:
Goodman SM, Mehta BY, Zhang M, Szymonifka J, Nguyen JT, Lee YY, Figgie MP, Parks ML, Dey SA, Crego DB, Russell LA, Mandl LA, Bass AR. Social Factors and Racial Disparities in Total Hip Arthroplasty Outcomes [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/social-factors-and-racial-disparities-in-total-hip-arthroplasty-outcomes/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/social-factors-and-racial-disparities-in-total-hip-arthroplasty-outcomes/
