Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Sleep disorders and fatigue are common in children with chronic pain syndromes, and contributes to psychosocial dysfunction, healthcare utilization, and school absences. We hypothesize that pediatric patients with chronic pain who are treated in an interdisciplinary pain rehabilitation program (IPRP) will have significant self-report of fatigue and sleep disturbance at baseline that will be corroborated by physiological evidence using actigraphy. We postulate that self-report measures and sleep physiology will improve after program completion.
Methods: This is a prospective longitudinal study of adolescents with chronic pain who completed an IPRP. This outpatient program provides daily intensive physical and occupational therapy, sleep education, self-regulation training, and behavioral health intervention. All pain and sleep medications are discontinued prior to program entry. 20 patients (16 female) age 12-18 with chronic musculoskeletal pain were evaluated at baseline, weekly during treatment, and again at 1-month after program completion by self-report PROMIS measures of fatigue and sleep disturbance (including items assessing sleep satisfaction and insomnia), and by actigraphy using Motionlogger watches. Paired samples t-tests were conducted with SPSS (V.23) and supplemented with hierarchical linear modeling (HLM7) for time-series analyses.
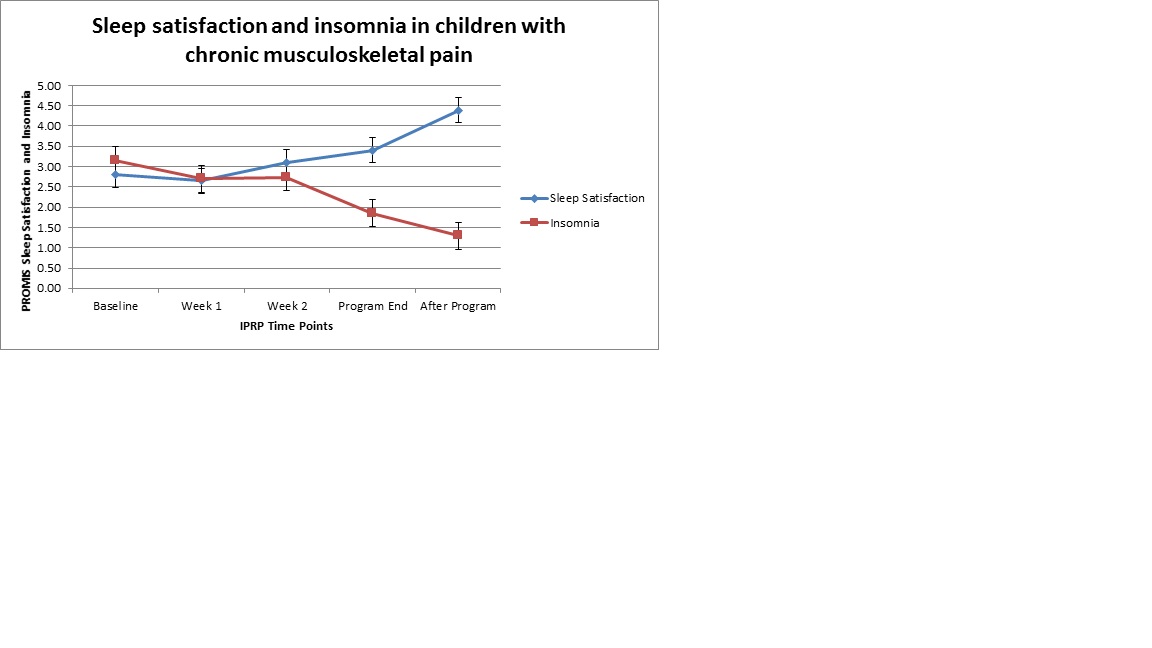
Results: Participants report difficulty falling asleep at baseline with insomnia score of 3.15 on a scale of 1 to 5. They are unsatisfied with sleep, with a score of 2.80. Both insomnia and sleep satisfaction significantly improve by program end (P<0.001), with continued improvement to 1.29 and 4.39 (P<0.001), respectively at 1-month follow-up. At baseline, patients report high daytime fatigue 24.30 on a scale of 0 to 40 and sleep disturbance 31.65 on a scale of 8 to 40. Both of these measures improved significantly, with fatigue changing from significantly impaired to normal (8.43, P<0.001) at 1-month follow-up. Actigraphy showed improvement in total minutes asleep after the first week (P=.02) and this was maintained at program end (P=.03), but not in the weeks after the program (P=.21). Sleep efficiency, sleep latency, and duration of first sleep episode did not show significant change during the program.
Conclusion: Children with chronic musculoskeletal pain report severe sleep impairments prior to starting an intensive pain rehabilitation program. Following the program they report significant improvements with insomnia, sleep satisfaction, daytime fatigue, and sleep disturbance. Despite statistically significant change in all patient-reported outcomes, these findings are not mirrored by objective data using actigraphy. Long-term follow-up and a larger sample size is needed to determine whether these outcomes will eventually more closely match patient report, or whether subjective issues are the most important improvement.
To cite this abstract in AMA style:
Hoffart C, Fortney S, Wallace D. Sleep Disruption in Children with Chronic Pain [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/sleep-disruption-in-children-with-chronic-pain/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sleep-disruption-in-children-with-chronic-pain/