Session Information
Date: Monday, November 6, 2017
Title: Systemic Lupus Erythematosus – Human Etiology and Pathogenesis Poster I
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose : Systemic Lupus Erythematosus (SLE) is a clinically diverse disease with a complicated pathophysiology highlighted in part by interferon (IFN) pathway dysregulation. Recent studies demonstrated that most pediatric SLE patients exhibit unabated IFN activities measured by microarray transcriptional scores. This study assessed the prevalence of these IFN active modules in adult SLE and determined association of these IFN active modules with lupus clinical features.
Methods: Gene expression profiles and associated IFN activities (IFN) of whole peripheral blood from 176 SLE patients who met ACR disease classification criteria were evaluated using modular transcriptional analysis based on Illumina Beadchip microarray data per (PMC2727981). ACR criteria and sub-criteria, clinical manifestations, co-morbidities, and autoantibody positivity history were extracted from medical records by rheumatology trained investigators using a standard protocol. Lupus Severity Index (LSI) was calculated by two methods (Katz: 8330033; Montgomery: PMC4800735). Proportionality, chi-square, and mixed conditional logistic regression tests were used to analyze prevalence differences as well as to detect co-variate effects among different populations.
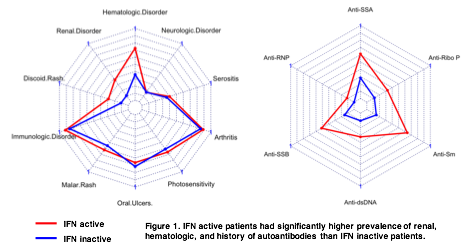
Results : One hundred patients were found to have active IFN pathways, while 76 patients had inactive IFN pathways by gene expression modules. Gender and ethnicity were not associated with IFN activation status in this adult SLE population. Patients with active IFN (mean: 29, range: 22 Ð 44) had earlier disease onset than patients with inactive IFN (37.5, 28 Ð44; p<0.05). Patients with inactive IFN were more likely to report myalgias (68.7% vs 42.5%; Odds Ratio, 2.04) and arthralgias (79.1% vs 60%; OR, 3.23) compared to IFN active patients (p<0.05). However, hematologic (72.5% vs 35.8%; OR, 4.76; p<0.001) and renal (37.5% vs 10.4%; OR, 5.00; p<0.001) criteria were more common in IFN active patients. IFN active patients were also more likely to have autoantibody specificities to dsDNA (61.3% vs 28.5%; OR, 2.78; p<0.01), RNP (51.3% vs 14.9%; OR, 5.88; p<0.01), Ro (63.8% vs 14.9%; OR, 3.57; p<0.01), Sm (32.5% vs 10.4%; OR, 4.17; p<0.01), La (33.0% vs 11.9%; OR, 10.00; p<0.01), and Ribosomal P (11.3% vs 0.00%; OR, N/A; p<0.01) compared to IFN inactive patients. Overall, SLE patients with active IFN had higher Montgomery LSI [5.44, (4.65 Ð 5.65) vs 5.07, (4.43 Ð 5.65); p<0.05] and Katz LSI [4, (2.75 Ð 6.00) vs 2, (1.5 Ð 3.5); p<0.001] than IFN inactive patients.
Conclusion: In the current study, 57% of adult SLE patients had active IFN pathways and these patients were more like to have renal, hematologic, and immunologic involvement compared to IFN inactive patients and scored higher on both SLE disease severity indices.
To cite this abstract in AMA style:
Lu R, Guthridge JM, Arriens C, Aberle T, Kamp S, Munroe ME, Gross T, DeJager W, Macwana S, Roberts VC, Apel S, Chen H, Gurung H, Chakravarty E, Thanou K, Merrill JT, James JA. SLE Patients with Active Interferon Pathways Showed More Systemic Disease Involvement Than Patients with Inactive Interferon Pathways [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/sle-patients-with-active-interferon-pathways-showed-more-systemic-disease-involvement-than-patients-with-inactive-interferon-pathways/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sle-patients-with-active-interferon-pathways-showed-more-systemic-disease-involvement-than-patients-with-inactive-interferon-pathways/