Session Information
Session Type: Abstract Session
Session Time: 4:00PM-5:30PM
Background/Purpose: SLE patients have increased rates of HPV infection and cervical cancer. Although some factors are recognized for HPV infection in SLE, the relationship with SLE disease activity is not well studied. Here, we studied the association between SLE activity and HPV infection in a time adjusted manner.
Methods: We studied patients visiting lupus clinic between May 2020 and May 2022. We included females between 21 to 65 years who had at least 1 pap smear after SLE diagnosis. Patients who had hysterectomy were excluded. We collected HPV vaccination data, HPV results, disease activity and exposure to immunosuppression since 2011.
SLE Disease Activity Index 2000 (SLEDAI-2K) and prednisone doses were recorded for each visit. Time adjusted SLEDAI (TAS) and time adjusted prednisone dose (TAP) were determined by calculating the area under the curve of over time. Data for 3 consecutive clinic visits were used.
Immunosuppressive drugs were divided into 3 groups: Conventional: Methotrexate; nonbiologic: Azathioprine, Mycophenolate mofetil, Tacrolimus, Voclosporin, Cyclophosphamide; and biologic: Belimumab, Rituximab or Abatacept.
Descriptive statistics, univariate and multivariate logistic regression were performed.
Results: We studied 74 female SLE patients (61% Hispanic, 24% African American, and 15% Caucasian) who had no history of prior HPV. Only 3 patients had received HPV vaccine. The mean ± SD age was 41 ±11 years. The mean ± SD of SLE disease duration was 7.9 ± 4.3 years. The mean number of pap smears per patient was 2.6.HPV testing was performed on 68 patients and 19 patients were HPV positive. In 6 patients, HPV testing was not performed due to HPV screening guidelines. The average time between visits was 3.7 months. The mean ± SD TAS and TAP were 4.2± 3.7 and 7.7 ± 13.1 mg, respectively.
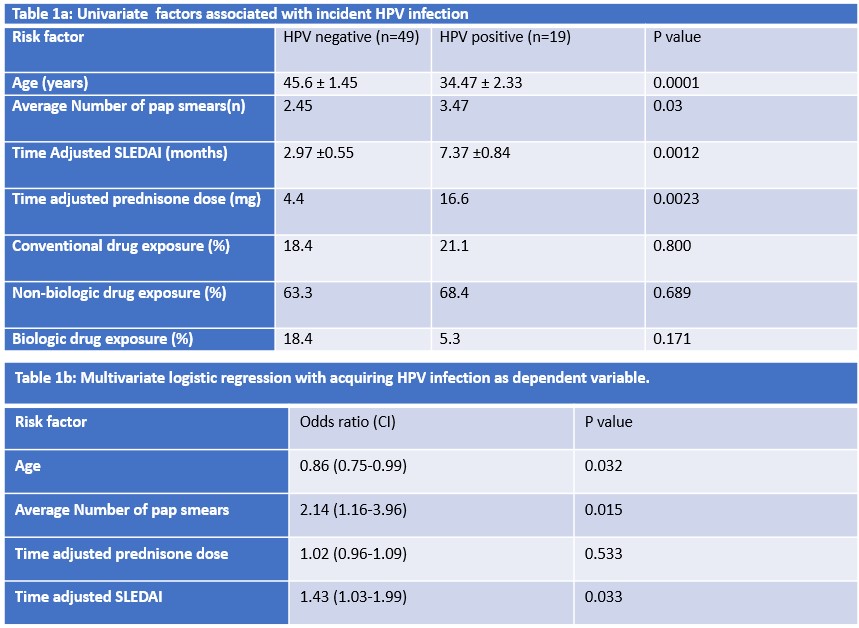
In univariate analysis, the risk of acquiring HPV was associated with younger age, higher number of pap smears, greater TAP dose, and higher TAS (Table 1a).The odds of acquiring HPV increase by 7.5% for 1 mg increase of TAP (OR 1.07, 95% CI: 1.01- 1.14). Ethnicity, SLE disease duration, alcohol use, hormonal contraception use and prior immunosuppression exposure were not associated HPV (p >0.05).
In multivariable logistic regression, age, number of pap smears and TAS were independently associated with HPV (p< 0.05 for all), but TAP was not (Table 1b). Patients were stratified into 3 TAS categories: mild < 3, moderate 3-6 and severe >6. Patients with severe SLE activity had 22.0 times higher odds of having HPV than those with mild activity (OR 22.0, 95% CI: 3.6-132.7, p 0.0007).
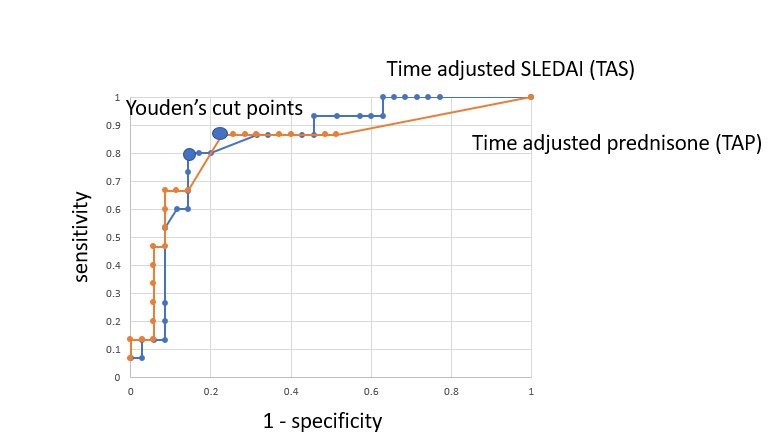
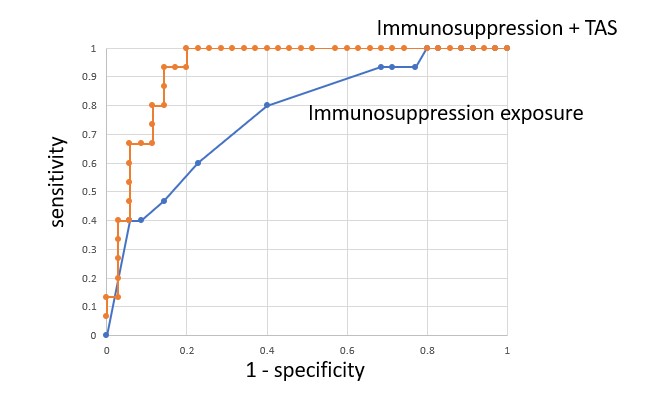
The cut point that better discriminated the risk of HPV infection for TAS was >5 (OR 24.0, 95% CI: 4.9-116.5) and for TAP was >15 mg (OR 16.0, 95% CI 3.5-72.6) (Figure 1). TAS increased the accuracy of immunosuppression exposure to detect HPV infection (Figure 2).
Conclusion: Our findings suggest that SLE disease activity is an independent risk factor for HPV infection, which has not been previously recognized. Reducing disease activity rather than immunosuppression may be the clinical approach to lower the risk for HPV infection. The biological basis for this association represents an important area for future study as is the role of disease activity in other infections among SLE patients.
To cite this abstract in AMA style:
Kazmi Z, Lorenzo C, Escalante A. SLE Disease Activity Is a More Important Risk Factor Than Immunosuppression for Acquiring Human Papillomavirus (HPV) Infection in Systemic Lupus Erythematosus Patients [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/sle-disease-activity-is-a-more-important-risk-factor-than-immunosuppression-for-acquiring-human-papillomavirus-hpv-infection-in-systemic-lupus-erythematosus-patients/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sle-disease-activity-is-a-more-important-risk-factor-than-immunosuppression-for-acquiring-human-papillomavirus-hpv-infection-in-systemic-lupus-erythematosus-patients/