Session Information
Date: Monday, November 6, 2017
Title: Systemic Lupus Erythematosus – Clinical Aspects and Treatment Poster II: Damage and Comorbidities
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Cardiovascular disease (CVD) is a leading cause of mortality in SLE and identifying those at risk remains challenging. While in the general population the Framingham Risk Score (FRS) and high-sensitivity CRP (hsCRP) are good predictors of CVD, in SLE their value remains controversial due to the known underperformance of the FRS and the variability of hsCRP levels. Interestingly high prevalence of nonspecific ST-T segment (NST-T) abnormalities was noted in an SLE inception cohort. While in the general population NST-T abnormalities are associated with increased risk of cardiovascular events, in SLE this association remains unknown. Therefore, we sought to identify SLE characteristics associated with the modified FRS (mFRS) as a surrogate outcome for CVD, with a particular interest in NST-T and hsCRP.
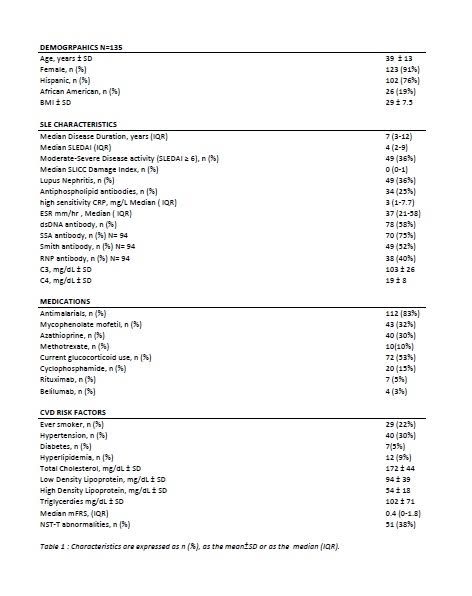
Methods: Adult SLE patients without clinical CVD continuously seen at a University Lupus Center between April 2016 and March 2017, meeting 1997 ACR classification criteria for SLE were studied. Patient characteristics including demographics, SLE-specific features, medication use, traditional CVD risk factors, 12-lead electrocardiogram (EKG), and hsCRP , were ascertained. High-level hsCRP was defined as ≥75th percentile. Univariable and multivariable linear regression models were constructed to test the association of NST-T and high-level hsCRP with the mFRS.
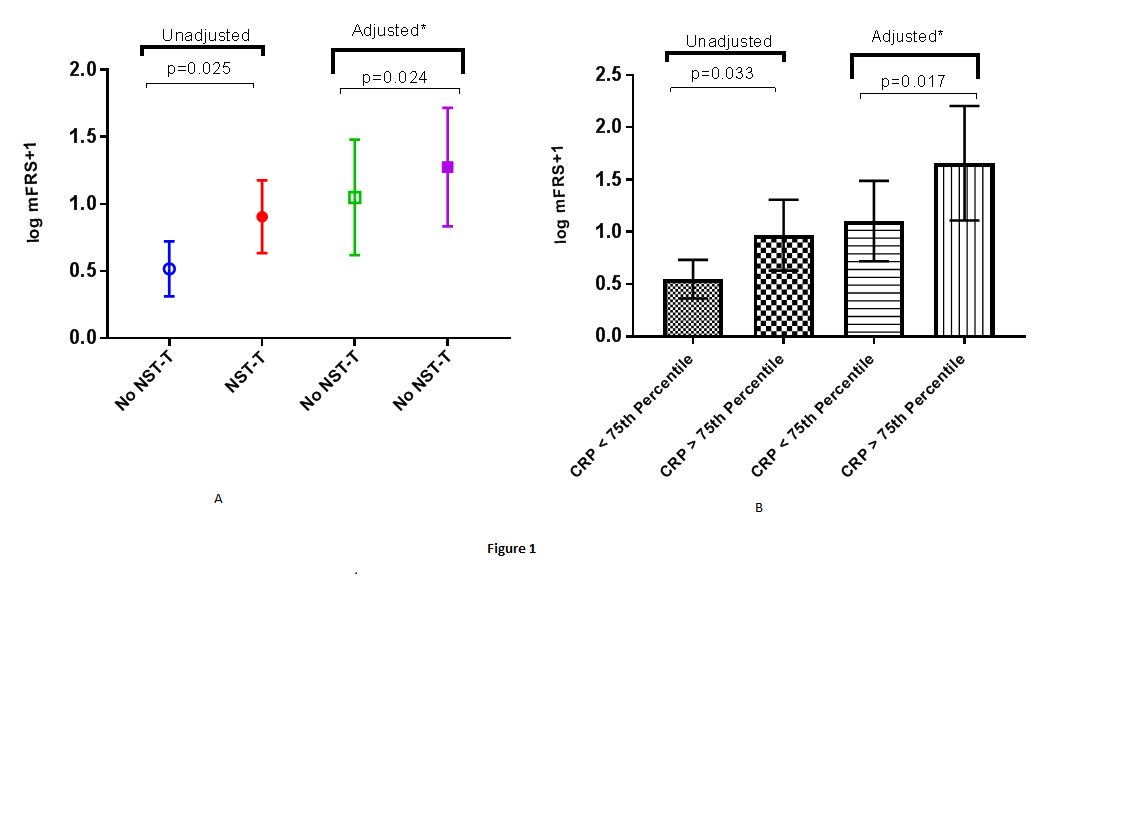
Results: One hundred and thirty five SLE patients (baseline characteristics in table 1) were studied. In univariable analyses, presence of NST-T abnormalities (0.389, p=0.025), high-level hsCRP (0.421, p=0.033), and the SLICC/ACR Damage Index (SDI) ( 0.24, p=0.004) were significantly associated with a higher mFRS. After adjusting for variables associated with NST-T abnormalities, hsCRP, and the SDI, respectively, including total protein, Female sex and use of methotrexate these associations remained statistically significant (NST-T:0.816,p=0.024; hsCRP75:0.527,p= 0.017; and SDI:0.193, p=0.016)(Figure 1).
Conclusion: EKG nonspecific ST-T abnormalities, high-level hsCRP and the SDI are all independently associated with a higher mFRS in SLE patients without clinical CVD.
To cite this abstract in AMA style:
George E, Perez T, Perez N, Askanase A, Geraldino-Pardilla L. SLE Characteristics Associated with Modified Framingham Risk Score in Patients without Clinical Cardiovascular Disease [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/sle-characteristics-associated-with-modified-framingham-risk-score-in-patients-without-clinical-cardiovascular-disease/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sle-characteristics-associated-with-modified-framingham-risk-score-in-patients-without-clinical-cardiovascular-disease/