Session Information
Date: Friday, November 6, 2020
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: The degree of joint and skin involvement varies across patients with PsA. Differences in patient outcomes with active joint only vs. joint plus skin involvement have not been extensively studied in a real-world setting. The objective of this study was to assess prevalence of joint-only and joint-plus-skin disease in a real-world clinical setting, and to assess the incremental impact of skin symptoms on quality of life (QoL), disability and work productivity.
Methods: A cross-sectional survey in patients with PsA recruited by rheumatologists and dermatologists was conducted in France, Germany, Italy, Spain, UK and US. Data were collected Jun-Aug 2018 via physician-completed forms and patient-completed forms. Patients were compared by joint and skin involvement (joint only, joints plus 1-3%, >3-10%, and >10% body surface area [BSA]) using parametric and non-parametric tests. Multiple linear regression analyses examined impact of incremental BSA on patient reported outcomes (PROs) (EQ5D, HAQ-DI, PsAID12, WPAI). Models controlled for gender, age, time since diagnosis, employment status, biologic DMARD use, BMI, number of joints affected.
Results: Of 1,909 patients (539 US, 1,370 EU), 35% of patients had joint-only disease, while 26%, 23%, and 16% experienced joint disease plus 1-3%, >3-10%, and >10% BSA respectively (Figure 1). Patients were comparable demographically (Table 1). After controlling for demographics and number of joints involved, results showed BSA independently and significantly impacted QoL, work productivity, disability (Table 2).
Conclusion: Two thirds of this sample of actively treated PsA patients had skin involvement. Over half had moderate-severe psoriasis (BSA >3%). Joint counts increased with BSA. After controlling for joint counts, increasing skin involvement adversely impacted QoL, disability and work productivity.
 Figure 1: Prevalence of joint and skin involvement across regions.
Figure 1: Prevalence of joint and skin involvement across regions.
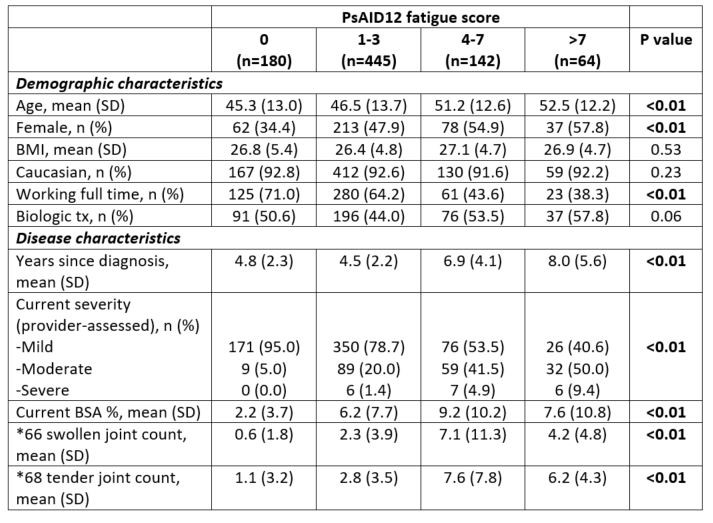 Table 1: Comparison of patient demographic and disease characteristics by joint and skin disease involvement. *Calculated on available data, n=394.
Table 1: Comparison of patient demographic and disease characteristics by joint and skin disease involvement. *Calculated on available data, n=394.
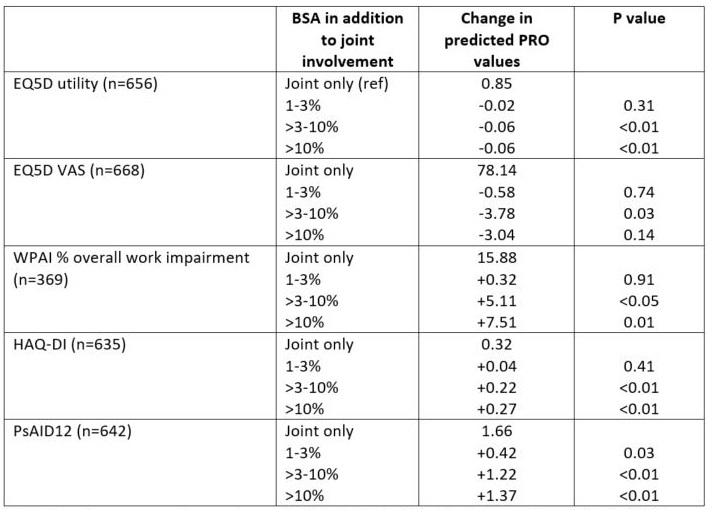 Table 2: Incremental impact of BSA on PROs. α PRO key for worse outcome (range): EQ5D utility (0-1.0) = lower; EQ5D VAS (1-100) = lower; WPAI (0-100) = higher; HAQ-DI (0-3) = higher; PsAID12 (0-10) = higher.
Table 2: Incremental impact of BSA on PROs. α PRO key for worse outcome (range): EQ5D utility (0-1.0) = lower; EQ5D VAS (1-100) = lower; WPAI (0-100) = higher; HAQ-DI (0-3) = higher; PsAID12 (0-10) = higher.
To cite this abstract in AMA style:
Walsh J, Ogdie A, Michaud K, Peterson S, Holdsworth E, Meakin S, Chakravarty S, Booth N, Schubert A, Piercy J, Gossec L. Skin Involvement in Psoriatic Arthritis (PsA) – The Incremental Impact of Psoriasis on Quality of Life, Disability and Work Productivity: Real-world Survey in US and Europe [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/skin-involvement-in-psoriatic-arthritis-psa-the-incremental-impact-of-psoriasis-on-quality-of-life-disability-and-work-productivity-real-world-survey-in-us-and-europe/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/skin-involvement-in-psoriatic-arthritis-psa-the-incremental-impact-of-psoriasis-on-quality-of-life-disability-and-work-productivity-real-world-survey-in-us-and-europe/
