Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Sjӧgren’s syndrome (SS) is the second most common systemic autoimmune disease, typically characterized by ocular and oral sicca. SS is associated with reduced quality of life and increased costs, but the contribution of oral symptoms to morbidity is unclear. The Sjӧgren’s Syndrome Foundation conducted a national survey of 2,962 adults with SS. We hypothesized that oral symptoms of SS predict reduced quality of life and financial burden in SS.
Methods: Methods: This survey included adults with self-reported SS. Oral symptoms/signs were assessed by frequency (never to daily) of eight categories: parotid swelling, dry mouth, oral ulcers, oral candidiasis, dysphasia (“trouble speaking”), dysphagia, sialolithiasis/gland infection, and caries. We calculated the prevalence of oral symptoms/signs (classified as present if symptoms occurred ≥ monthly) and current/ever use of oral treatments. We performed multivariable logistic regression to evaluate the association between oral symptoms (predictor) and quality of life and financial burden (outcome variables), adjusted for age, sex, race, and employment. Binary (present = “a lot of negative impact” or “a great deal of negative impact”; absent = no or “some negative impact”) quality of life/financial burden outcomes included: 1) challenge of living with SS, 2) financial burden, 3) activities of daily living (ADLs), and 4) ability to work.
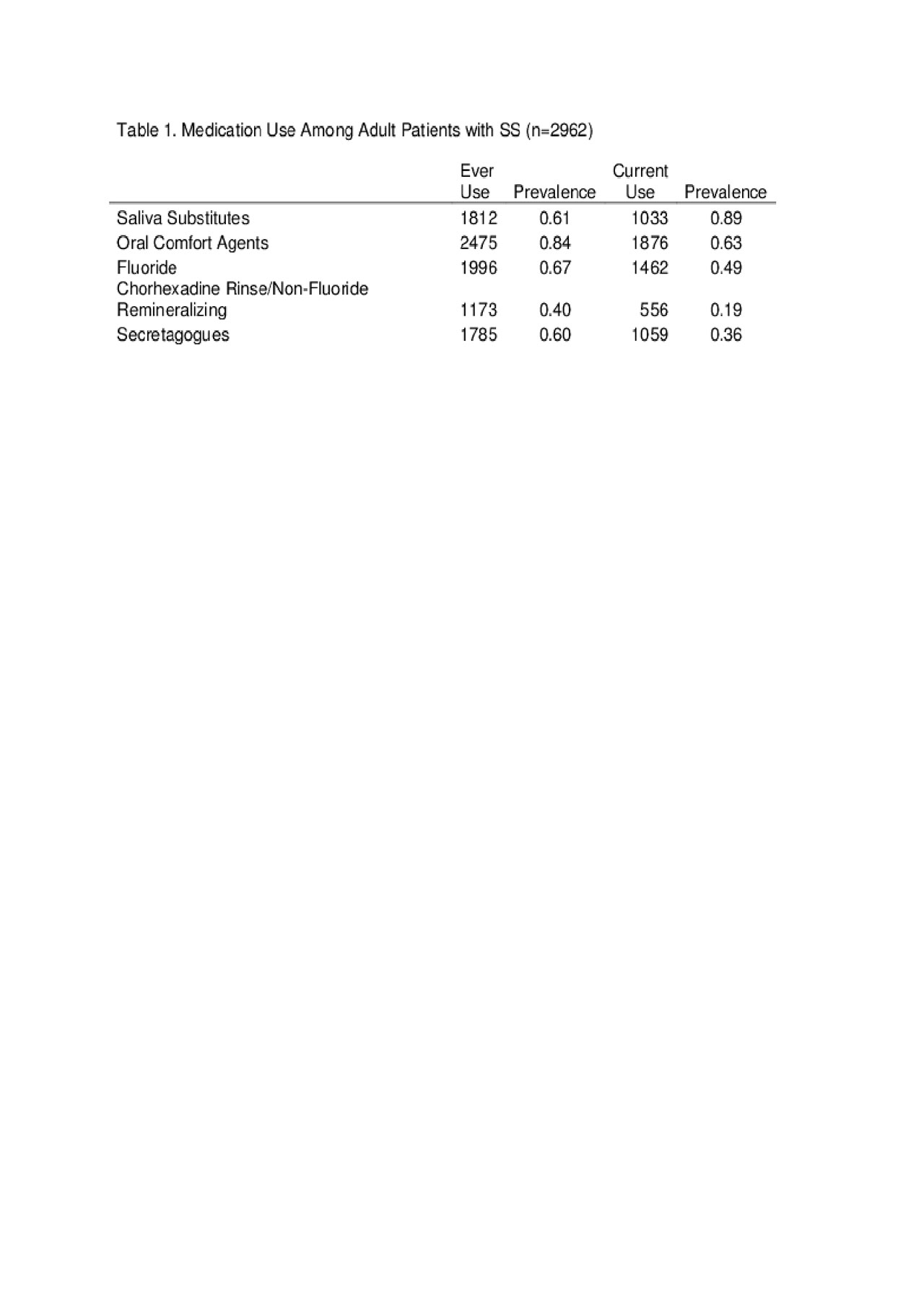
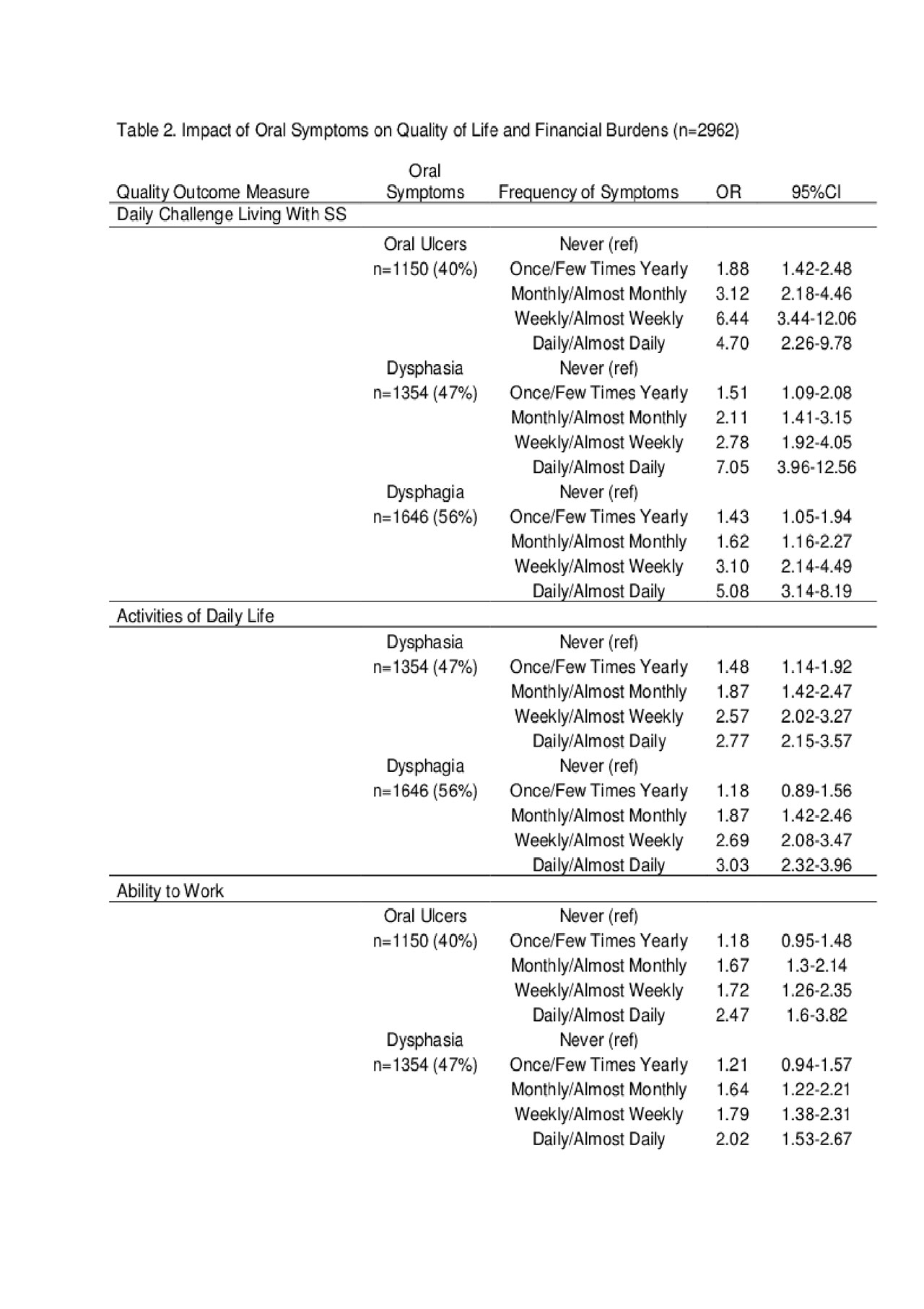
Results: The 2,962 survey participants were 92.6% white, 95.6% female, and averaged 65.1 years of age. Most respondents had dry mouth (96.5%) followed by dysphagia (57.5%), dysphasia (47.0%), oral ulcers (40.0%), caries (22.4%), parotid swelling (17.7%), oral candidiasis (8.8%), and sialolithiasis/gland infection (3.8%). Eighty-four percent of respondents used oral comfort agents, 67% used fluoride, and 60% used secretagogues previously, but less than half currently use fluoride and secretagogue treatment (Table 1). Significant dose dependent relationships between frequency of oral symptoms quality of life/financial burden measures were observed. Dysphasia impacted all four quality/financial measures including daily living challenges (OR 7.05 [95% CI 3.96-12.56), ADLs (OR 2.77 [95%CI 2.15-3.57), work ability (OR 2.02 [95% CI 1.53-2.67]), and financial burden (OR 3.08 [95% CI 2.34-4.06]) (Table 2). Oral ulcers and dysphagia impacted three of four quality/financial measures (Table 2).
Conclusion: Oral symptoms occurred in the majority of SS respondents, yet less than half of respondents remain on secretagogue or fluoride therapies. This lack of persistence might reflect reduced perceived symptomatic benefits or cost burdens of SS. Dysphasia impacted all four outcome categories in a dose dependent manner by symptom frequency with up to a seven fold odds increase in the challenges with daily living. Dysphasia, oral ulcers, and dysphagia most strongly impacted multiple quality of life measures compared to other oral aspects, potentially identifying dysphasia, oral ulcers, and dysphagia as important but underutilized patient reported outcome measures. Furthermore, these findings highlight the potential importance of targeted treatment toward dysphasia and dysphagia.
To cite this abstract in AMA style:
McCoy S, Bartels C, Akpek E, Saldanha I, Bunya V, Makara M, Baer A. Sjӧgren’s Syndrome Foundation National Survey: The Impact and Burden of Oral Symptoms [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/sj%d3%a7grens-syndrome-foundation-national-survey-the-impact-and-burden-of-oral-symptoms/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sj%d3%a7grens-syndrome-foundation-national-survey-the-impact-and-burden-of-oral-symptoms/