Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with rheumatoid
arthritis (RA) have an excess risk of cardiovascular disease (CVD). There is a
clear female to male preponderance of RA. In the general population it is well
documented that females have their CVD diagnosed at a later stage compared to
males. We therefore evaluated if CVD risk prediction and CVD event rates
differed between females and males with RA, and if adjustments for traditional
and RA specific risk factors were of importance regarding sex differences in
CVD event rates.
Methods: RA cohorts from 13 rheumatology
centers were compared. Data on CVD risk factors and RA characteristics were
collected at baseline for each cohort; CVD outcomes (myocardial infarction, angina,
revascularization, CVD death, stroke and peripheral vascular disease) were
collected using standardized definitions. Standardized incidence ratios (SIR) (observed/expected
CVD event) were calculated with respect to sex using the following risk calculators
FRS, SCORE, ACC/AHA and QRISK II. The CVD-free survival between the sexes was compared
using adjusted Kaplan-Meier plots.
Results: 5638 patients with RA and
no prior CVD were included (mean age: 55.3 [SD: 14.0] years, 76% female).
During a mean follow-up of 5.8 (SD: 4.4) years, 437 patients developed CVD
events. Male patients had a significantly higher burden of traditional CVD risk
factors, including increased blood pressure, higher total cholesterol and were
more frequently smokers (p<0.001 for all).
Female RA patients used more anti-rheumatic medication, both synthetic and
biologic disease modifying anti-rheumatic drugs (p<0.001). Erythrocyte
sedimentation rate was higher in females, while C-reactive protein (CRP) levels
were highest in males (p<0.001 for both). SIRs (95% CI) using the various
CVD risk calculators were for females and males: FRS: 1.02 (0.80, 1.31) and
0.86 (0.67, 1.12) (p=0.19), SCORE: 0.34 (0.17, 0.67) and 0.25 (0.11, 0.58)
(p=0.98), ACC/AHA: 0.72 (0.50, 1.04) and 0.56 (0.36, 0.88) (p=0.74) and QRISKII
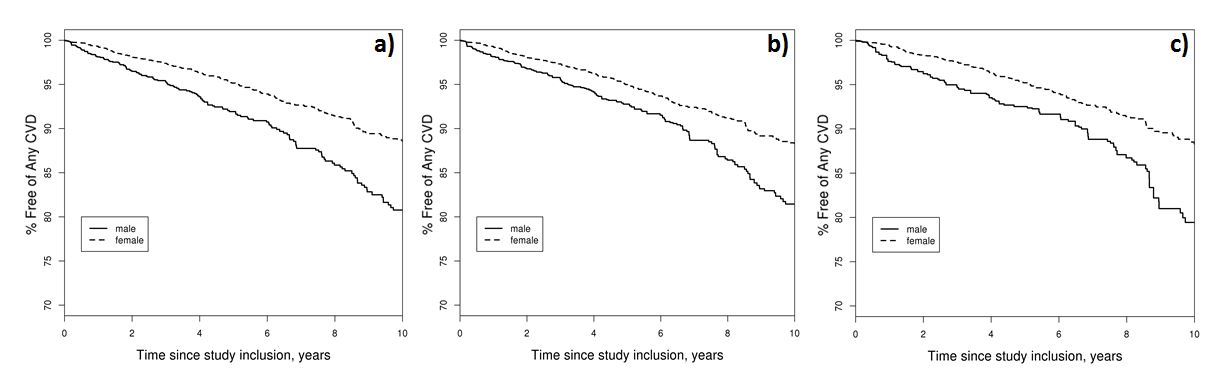
0.61 (0.47, 0.79) and 0.52 (0.35, 0.79) (p=0.42). The 10 year CVD-free survival
differed significantly between the sexes, both when adjusting for a) age, b)
age and CVD risk factors and c) age, CVD risk factors and RA disease
characteristics (Females [mean %±SD] 88.3±0.3, males 79.4±0.4), p<0.001 for
all (Figure 1).
Conclusion:
In a large
international cohort of patients with RA, there was no sex difference in the
ability of the various risk calculators to predict CVD. However, the FRS seems
to predict CVD risk more accurately compared to the other risk calculators in both
sexes. CVD-free survival was significantly higher in females, even after
adjustments for both traditional and RA specific risk factors.
Figure 1. Kaplan Meier plots for CVD-free survival by sex in
patients with rheumatoid arthritis
To cite this abstract in AMA style:
Rollefstad S, Ikdahl E, Crowson CS, Gabriel S, Kitas GD, van Riel PL, Semb AG. Sex Differences in Cardiovascular Risk Factors and Event Rates in Patients with Rheumatoid Arthritis – Data from 13 Rheumatology Centers [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/sex-differences-in-cardiovascular-risk-factors-and-event-rates-in-patients-with-rheumatoid-arthritis-data-from-13-rheumatology-centers/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sex-differences-in-cardiovascular-risk-factors-and-event-rates-in-patients-with-rheumatoid-arthritis-data-from-13-rheumatology-centers/