Session Information
Date: Monday, October 22, 2018
Title: Systemic Lupus Erythematosus – Etiology and Pathogenesis Poster II
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: SLE is a clinically heterogeneous disease oftentimes characterized by a waxing and waning course. Mechanisms of SLE flare remain elusive. This study examined relationships between SLE disease activity, immune pathways and serologic evidence of viral exposures and reactivation in molecular subsets of SLE patients.
Methods: Serial or single samples of plasma and RNA (n=290) were collected from 184 adult SLE patients who met ACR classification and cohort matched controls (n=49). Disease activity was assessed by the SELENA- modified SLEDAI. Immune pathways were evaluated by modular transcriptional analysis of gene expression data (Illumina Beadchip) and by soluble mediators (n=32; multiplex bead-based assay and ELISAs). These data were used in random forest modeling to group patients into seven molecular defined subsets. Viral seropositivity and antibody concentrations were detected by ELISA for antibodies against Epstein Barr virus (EBV)-Viral Capsid Antigen (VCA; IgG and IgA), EBV-Early Antigen (EA; IgG), Cytomegalovirus (CMV; IgG), and Herpes Simplex Virus (HSV1; IgG).
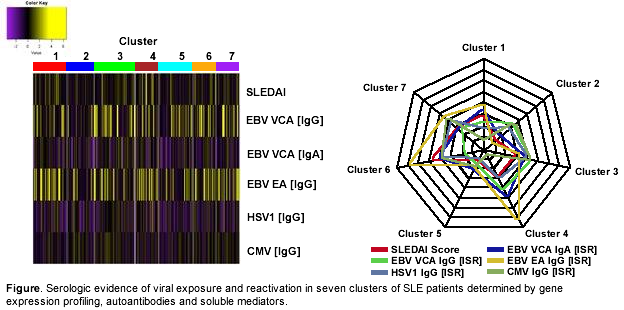
Results: Serologic evidence of EBV reactivation was more common in SLE patients versus controls as measured by antibodies against EBV-EA (IgG; 40% vs 13%; OR=4.57, p=0.0006) or EBV-VCA (IgA; 36% vs 17%; OR=2.70, p=0.019). CMV1 and HSV1 seropositivity rates showed no differences between patients and controls. IgG responses against EBV-VCA were nearly universal in these adult patients and controls, but concentrations of EBV-VCA (IgG and IgA) and EBV-EA (IgG) were higher in SLE patients (Table). In cross sectional analysis SLE patients with higher disease activity had higher concentrations of EBV-EA IgG than those with lower disease activity (Table). SLE patients with serologic evidence of EBV reactivation by EA IgG responses had higher levels of interferon (IFN) associated molecules IP10 (p=3.4 X 10-14), BLyS (5.5 X 10-5), and IL10 (p=0.00013). HSV1 IgG positive SLE patients also showed higher levels of IP10 (2.2 X 10-7). EBV-EA IgG responses were enriched in molecularly defined patient clusters with higher expression of IFN and inflammatory modules and soluble mediators (Figure). Patients in these clusters were also more likely to have major organ involvement, such as renal or neurologic disease.
Conclusion: Serologic evidence of EBV reactivation is more common in SLE patients compared to healthy controls. EBV-EA IgG is elevated in SLE patients with active disease and corresponds with increases in IFN-associated mediators. This study provides serologic evidence suggesting a possible role for viral reactivation in SLE disease activity.
To cite this abstract in AMA style:
Wood R, Guthridge L, Guthridge CJ, Bourn RL, Chen H, DeJager W, Macwana SR, Kamp S, Lu R, Arriens C, Chakravarty E, Thanou K, Merrill JT, Guthridge JM, James JA. Serologic Evidence Linking Epstein Barr Virus Reactivation, Heightened Interferon Pathway Activation and Increased Disease Activity in Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/serologic-evidence-linking-epstein-barr-virus-reactivation-heightened-interferon-pathway-activation-and-increased-disease-activity-in-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/serologic-evidence-linking-epstein-barr-virus-reactivation-heightened-interferon-pathway-activation-and-increased-disease-activity-in-patients-with-systemic-lupus-erythematosus/